Fatigue Sleep Quality and Disability in Relation to Quality of Life in Multiple Sclerosis
Original Article
Fatigue, Sleep Quality, and Disability in Relation to Quality of Life in Multiple Sclerosis
Fatemeh Moghaddam Tabrizi, PhD; Moloud Radfar, PhD
Journal of International MS Care
Background: Quality of life (QOL) is impaired in multiple sclerosis (MS) in part due to physical disability. MS-associated fatigue and poor sleep are common and treatable features of MS that affect QOL. We assessed the association between fatigue, sleep quality, and QOL in people with MS.
Methods: Cross-sectional data were collected from 217 patients with MS. Health-related QOL (MS Quality of Life-54), fatigue (Fatigue Severity Scale [FSS]), and sleep quality (Pittsburgh Sleep Quality Inventory [PSQI]) were assessed. Expanded Disability Status Scale scores were also provided by a qualified neurologist.
Results: The mean ± SD age of the 217 patients was 32.6 ± 8.6 years, and 79% were female. One hundred fifty-two patients (70.0%) were classified as poor sleepers based on PSQI scores; 122 (56.2%) had significant fatigue based on FSS results. The mean ± SE physical (PCS) and mental (MCS) health composite scores of the MSQOL-54 were 40.12 ± 1.27 and 43.81 ± 1.61, respectively. There was a strong statistically significant positive correlation between PCS scores and MCS (r = 0.58), FSS (r = 0.49), and PSQI (r = 0.52) scores. MCS scores were strongly correlated with FSS (r = 0.53) and PSQI (r = 0.35) scores. Age exhibited statistically significant negative correlations with PCS (r = −0.21) and MCS (r = −0.58) scores, and was statistically significantly correlated with FSS (r = 0.23) and PSQI (r = 0.21) scores. Expanded Disability Status Scale scores were strongly correlated with FSS scores.
Conclusions: These findings support screening of fatigue severity and sleep quality and their effects on QOL.
Multiple sclerosis (MS) is a chronic, inflammatory, immune-mediated disease of the central nervous system that usually affects young adults, with a higher incidence in women. The mean annual MS incidence rate in Europe is 4.3 cases per 100,000.1 Quality of life (QOL) is substantially impaired in people with MS compared with the general population.2Studies have shown that individuals with MS have lower overall and disease-specific QOL scores than healthy individuals and populations with other chronic diseases, such as diabetes, epilepsy, and rheumatoid arthritis.3,4
Health-related QOL (HRQOL) is a multidimensional concept that includes self-reported physical, mental, emotional, and social functioning. The QOL scales have become very important as clinical trial outcome measures in MS.5 Recent studies have attempted to correlate advancing neurologic disability with impaired QOL in patients with MS.2Although some studies showed that QOL was correlated with disability,6 as measured by the Expanded Disability Status Scale (EDSS), most studies showed that disability status has a limited influence on QOL7 and only partly explains impaired QOL.8 This supports the hypothesis that other factors, including fatigue and poor sleep, may play a role in the QOL of patients with MS.
Fatigue is one of the most common symptoms in MS; it has been reported by 53% to 90% of patients. Chronic fatigue in MS is often rated by patients as one of the most disabling symptoms, with a great effect on QOL.9 Fatigue can be defined as uncontrollable apathy, lack of energy, or a feeling of exhaustion that cannot be fully explained by depression or muscle weakness. In two-thirds of patients with MS, it is ranked as one of the three main symptoms and one of the most troublesome symptoms of the disease.7 Patients are often unable to distinguish between fatigue (a subjective sense of decreased energy) and sleepiness due to sleep disturbance.
Patients with MS frequently report poor sleep, and sleep disorders are more common in patients with MS than in healthy individuals.10 Prevalence studies have shown that up to 54% of patients with MS may have significantly more sleep problems than the general population, including insomnia, nocturnal movement disorders, sleep-disordered breathing, narcolepsy, and rapid eye movement sleep behavior disorder.11,12 In one study, the prevalence of sleep concerns was three times greater in a group of patients with MS than in controls.13 Causes of poor sleep in MS are likely multifactorial, and may include adverse effects from immunotherapy and symptomatic medications, and MS-associated symptoms, such as pain, depression, and fatigue.11,14 Patients with a sleep disturbance have an increased risk of comorbid conditions such as heart disease, obesity, and diabetes that may have a profound effect on long-term health.15 It is generally considered that maintaining a good quality of sleep is very important for any individual, healthy or ill, because it significantly contributes to physical and emotional health and personal productivity.16
A chronic progressive disease such as MS can lead to the development of a considerable degree of emotional distress and decreased QOL in patients.17 Only a few authors have investigated the influence of disability, fatigue, and sleep disturbance associated with MS on QOL. The main goal of this study was to quantify QOL in a large community-based sample of individuals with MS using the Multiple Sclerosis Quality of Life–54 (MSQOL-54), a disease-specific instrument, and to assess its relationship with fatigue severity and sleep quality.
Materials and Methods
Patients
Two hundred seventeen consecutive patients referred to the MS association outpatient center in Urmia, in northwestern Iran, between March 1, 2013, and January 31, 2014, were included in the study. All the patients had a diagnosis of definite MS according to the McDonald criteria, and their EDSS scores18 were 6.0 or lower. Exclusion criteria were active infection, corticosteroid therapy in the past 2 weeks, treatment with amantadine, and antidepressant therapy initiated in the past 6 weeks.
Demographic data, including age, marital status, socioeconomic status, and education, were recorded. Clinical data concerning disease course and duration and EDSS scores were provided by a qualified neurologist. The study was approved by the ethics committee of Urmia University of Medical Sciences, Urmia, Iran. All the patients signed an informed consent form before data collection.
Instruments
Pittsburgh Sleep Quality Index
The Pittsburgh Sleep Quality Index (PSQI) measures subjective sleep quality with a recall period of 1 month. It consists of 19 self-rated questions and 5 questions rated by a bed partner or roommate (the last 5 questions are used for clinical information only and are not reported in this article). The 19 items are grouped into seven component scores: sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. These component scores are summed to obtain a global PSQI score ranging from 0 to 21, with higher scores indicating worse sleep quality. A global PSQI score of more than 5 has been suggested to distinguish poor sleepers (PSQI score >5) from good sleepers (PSQI score ≤5), with a diagnostic sensitivity of 89.6% and a specificity of 86.5%. The PSQI is well validated and has been widely used to study subjective sleep quality in healthy people and those with psychiatric and medical disorders, including MS.7 The Iranian version of the PSQI used in the present study has been shown to have high reliability of whole questions by the Cronbach alpha coefficient (α = 0.89).7
Fatigue Severity Scale
We used an Iranian version of the Fatigue Severity Scale (FSS), a 9-item scale that reflects how fatigue influences motivation, exercise, physical functioning, and daily activities, and interferes with work, family, and social life. It has been shown to have high reliability of whole questions by the Cronbach alpha coefficient (α = 0.96).19Participants were asked to read each statement of the questionnaire and choose the number that best described their degree of agreement, from 1 (strongly disagree) to 7 (strongly agree). The final score is the average of all item scores, ranging from 1 to 7. A higher score indicates more fatigue severity. The patients were asked to assess their fatigue during the preceding 2 months when filling out the questionnaire. The FSS has acceptable internal consistency, stability over time, and sensitivity to clinical change.20
MSQOL-54 Questionnaire
Health-related QOL was assessed using the disease-specific MSQOL-54 questionnaire.21 The MSQOL-54 consists of 54 items divided into 12 multi-item scales, 2 single-item scales, and 2 composite scores (physical and mental health). The subscales are as follows: physical function, role limitations–physical, role limitations–emotional, pain, emotional well-being, energy, health perceptions, social function, cognitive function, health distress, overall QOL, and sexual function. The summary scores are the physical health composite summary and the mental health composite summary. The MSQOL-54 has shown good reliability and validity in the MS population.22The Persian translation of the MSQOL-54 has been used for patients with MS and has proved to have high reliability of whole questions by the Cronbach alpha coefficient (α = 0.962).23 Scores for each dimension can range from 0 to 100 (full health). Scale scores are computed by averaging the items within scales and transforming the mean scores linearly, with possible scores of 0 to 100, with higher scores indicating better QOL. Physical and mental health composite scores were also calculated as a weighted sum of selected scales to generate a simplified two-factor solution to the MSQOL-54 instrument.24
Statistical Analyses
Descriptive statistics are reported as mean (±SE) for continuous variables, and as number (percentage) for categorical data. The Spearman correlation coefficient was used to test for any correlation between MSQOL-54 mental and physical summary scores and age, duration of disease, fatigue severity, and sleep quality. Data analyses were performed using a statistical software program (SPSS for Windows, version 15.0, SPSS Inc, Chicago, IL). A probability value of less than .05 was considered statistically significant.
Results
Demographic and Disease Characteristics
The mean ± SD age of the 217 respondents was 36.2 ± 8.6 years (range, 18.8–66.5 years); 91 patients (41.9%) were single, 120 (55.3%) were married, and 6 (2.8%) were divorced. The mean ± SD age at the onset of MS (time of diagnosis by medical professionals) was 31 ± 6.3 years. The duration of MS disease was 1 year or less in 95 patients (43.8%), 2 to 4 years in 85 (39.2%), and 5 years or longer in 20 (17.1%).
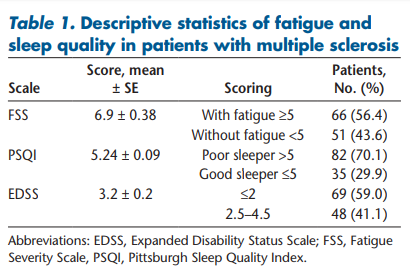
Sleep Quality, EDSS, and Fatigue Severity
Table 1 shows the mean ± SE PSQI global, EDSS, and FSS scores in patients. The mean ± SE PSQI score of the patient sample was 5.24 ± 0.09. Reduced sleep quality (PSQI score >5) was found in 82 patients (70.1%). The mean ± SE (FSS) score of the patient sample was 6.9 ± 0.38. We classified 51 patients (43.6%) as not having fatigue and 66 (56.4%) as having fatigue. Sixty-nine patients (59.0%) had EDSS scores of 2 or less, and the remaining 48 patients (41.0%) had EDSS scores of 2.5 to 4.5.
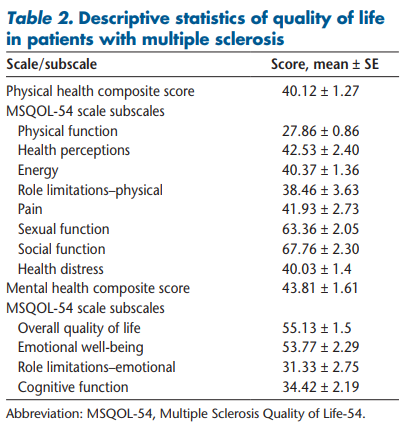
Quality of Life
The results of the QOL subscales are summarized in Table 2. The mean ± SE QOL physical and mental scores were 40.12 ± 1.27 and 43.81 ± 1.61, respectively. The participants achieved the highest and lowest mean ± SE scores in social function (67.76 ± 2.30) and physical function (27.86 ± 0.86), respectively, in all MSQOL-54 dimensions.
Sleep Quality, Fatigue Severity, EDSS Score, and Other Factors in Relation to QOL
Table 3 illustrates that there was a significant high positive correlation between the QOL physical score and the QOL mental score (r = 0.577, P < .01), fatigue (r = 0.486, P < .01), and sleep (r = 0.519, P < .001). There was a significant high positive correlation between the QOL mental score and fatigue (r = 0.531, P < .01) and sleep quality (r = 0.346, P < .01).
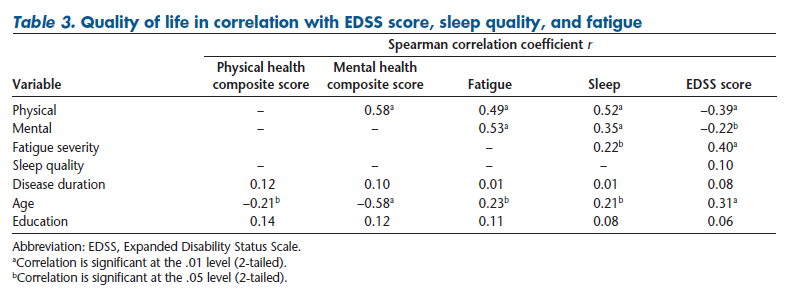
Similarly, there was a high positive correlation between EDSS score and fatigue (r = 0.40, P < .01) and a weaker but statistically significant negative correlation with the QOL mental and physical composite scores (r = −0.22, P < .01 and r = −0.39, P < .01, respectively). Age was negatively correlated with the QOL physical (r = −0.21, P < .05) and mental (r = −0.58, P < .01) composite scores and was significantly correlated with fatigue (r = 0.23, P < .05) and sleep quality (r = 0.21, P < .05). There was no significant correlation between the QOL composite scores and education or disease duration.
Discussion
Using the MSQOL-54, which includes additional questions about interpersonal function and social, emotional, personal, and spiritual fulfillment,6,22,23 we observed strong correlations between QOL, fatigue, and sleep quality in a relatively large sample of patients with MS treated in an outpatient MS center.
In the present study, the mean ± SE physical and mental summary scores of QOL were 40.12 ± 1.27 and 43.81 ± 1.61, respectively, consistent with the results published by Masoudi et al.25 (43.24 ± 2.79). Other studies from Iran reported higher mean ± SE QOL scores, including Taraghi et al.26 (50.41 ± 23.26) and Haresabadi et al.27 (56.2 ± 20.23). This small difference may be due to the higher mean ± SE age of the patients in this study (36.2 ± 8.6 vs. 33.2 ± 8.326and 33.3 ± 8.3,27 respectively). The QOL scores in patients with MS older than 65 years were reported in studies conducted in the United States, France, Spain, Italy, the Netherlands, and Turkey.2,28–30 Although it is difficult to ascertain the reasons for these differences, the low scores in the present patients underscore the need to enhance their QOL.
Generally, the present patients exhibited low scores on all the QOL subscales, with lower scores in the physical dimension compared with the mental dimension, consistent with findings from other studies.22,31 This can be explained by the negative impact of physical limitations from MS on the ability to fulfill roles such as functioning at work and social activities.5,32
In this study, there is a significant correlation (P < .001) between the physical and mental scores of QOL. This means that the reduction in QOL in the physical domain caused reduction in that in the mental domain. In the study by Ayatollahi et al.,33 a significant relationship was observed between psychological factors such as depression and physical health. The highest mean ± SE values of QOL were observed in domains of social function (67.76 ± 2.30), which is in agreement with the results of Haresabadi et al.27 and Taraghi et al.26
Most individuals in this patient sample reported fatigue as a disabling symptom. We classified 56.4% as experiencing fatigue. MS-related fatigue is likely to be associated with motor disturbances or mood disorders and to have an effect on QOL.34A major reason for fatigue is physical damage; damage to different regions of the brain can cause thinking and activities to require greater energy than before. On the other hand, spastic muscles can cause difficulties with physical activities. Demyelination makes it harder for neurons to send signals.35 In fact, the increase in neuronal activity in cellular tissues, which occurs to compensate for the problems, gradually leads to deterioration of physical abilities and subsequently results in depletion of the physical aspect of QOL in patients with MS.
The present study showed a strong correlation between fatigue severity and physical and mental QOL. The present findings were in line with most previous studies in that higher fatigue scores were associated with lower scores on all domains of QOL.7,36 Salehpoor et al.37 demonstrated that fatigue was identified as the physical component summary predictor variable, in agreement with the study by Turpin et al.,38 which revealed poorer physical HRQOL in those with greater fatigue.
These results show that fatigue can strongly influence the ability to perform daily activities and can become a major reason for unemployment.39 Also, it has been shown that the pressures cause changes in economic status, and struggling with this critical situation affects the QOL of patients with MS.40 Furthermore, it has been shown that psychological symptoms can affect self-efficacy and perception of self-worth in other patient populations41 because these symptoms can undermine the person's ability to cope.42 This situation can reduce the patient's QOL.
The present study showed a positive correlation between sleep quality and physical and mental QOL. This finding is supported by other researchers.10,31 There are few studies reporting on the impact of fatigue and sleep in patients with MS.8 In the present study, fatigue and poor sleep quality were strongly related. Several mechanisms may contribute to the relationship between fatigue and poor sleep in MS.43Increased levels of inflammatory cytokines or lesions in the brain may disrupt pathways involved with sleep. Sleep apnea, which is common in people with MS, may also result in fatigue and sleep disruption.15,44,45 Benedict et al.6reported that higher fatigue scores were associated with poor physical and mental summary scores. These findings highlight the importance of carefully screening all patients with MS for the presence of fatigue so that a variety of fatigue reduction strategies are implemented promptly.
The present study showed a strong significant positive correlation between physical and mental QOL and EDSS scores. This finding is in agreement with other studies.6,7Previous research has found patient physical disability to be associated with mental health challenges as well as reduced physical QOL.46,47 Interestingly, the present patient sample exhibited a relatively low level of neurologic disability, as measured by the EDSS, and most patients were within 5 years of symptom onset, demonstrating that QOL is significantly affected in the early stages of the disease. In addition, EDSS scores were significantly correlated with FSS scores but not with PSQI scores.
We found a negative correlation between age and either QOL dimension. Similarly, in a study by Krokavcova et al.,48increasing age was a significant predictor of worse perceived physical health status. Conversely, DiLorenzo et al.49concluded that the process of getting older enhances perceived mental health in MS. However, this positive association was observed in the group of individuals 65 years and older (compared with those aged 50–64 years), and this age group was not well represented in the present study. Education and disease duration were not associated with QOL, similar to the results of previous studies.31,48 In contrast, Buhse et al.47 showed that less education (high school or less, compared with at least some college) was negatively associated with mental HRQOL.
Some limitations of this study should be mentioned. First, the sample included patients from the western part of the country followed in one MS center; thus, the outcomes may not be representative of the whole MS population. To prevent such sample fluctuations, a large multicenter study is needed. Second, QOL could be related to other factors, including immunomodulatory or immunosuppressive treatment, cognitive dysfunction, social support, and employment status.48,50 These aspects have not yet been analyzed in this sample. In addition, mood alterations in the context of MS (particularly depression) were found to correlate with fatigue and QOL but were not assessed. Third, the study has a cross-sectional design, which does not provide us with information about changes in patients over time and thus does not allow us to explore causal pathways. Finally, we did not investigate the causes of sleep disturbance in the present patients.
Conclusion
In this study, both the physical and mental dimensions of HRQOL were found to be significantly associated with fatigue severity and sleep quality. These findings support the regular screening and monitoring of fatigue and sleep disturbance in patients with MS. Early detection and intervention may help improve patients' physical and mental HRQOL. Sleep disturbance is a potentially treatable condition. Increased awareness of modifiable risk factors for poor sleep in MS may be important for early therapeutic and prophylactic interventions. As suggested by Chervin,44 in patients with MS, individual symptoms, if left untreated, may worsen or precipitate other symptoms, producing a vicious circle. Consequently, disrupted sleep should be treated early, thus breaking this vicious circle and improving patients' mental and physical health status. Thus, the assessment of fatigue and sleep-related problems, and the determination of how a patient may be affected by these symptoms, have obvious clinical importance in the routine clinical evaluation of patients with MS.2,8 The present findings illustrate the need for a comprehensive approach to provide more adequate treatment strategies in order to achieve higher levels of health and QOL in patients with MS. Future research on fatigue and sleep quality in MS should consider exploring sleep disturbance in more detail, particularly its relationship with disease activity.
Acknowledgements
We thank the people with MS who participated in this study.
References
1. Koutsouraki E, Costa V, Baloyannis S. Epidemiology of multiple sclerosis in Europe: a review. Int Rev Psychiatry. 2010;22:2–13.
2. Janardhan V, Bakshi R. Quality of life and its relationship to brain lesions and atrophy on magnetic resonance images in 60 patients with multiple sclerosis. Arch Neurol. 2000;57:1485–1491.
3. Benito-León J, Morales JM, Rivera-Navarro J, Mitchell AJ. A review about the impact of multiple sclerosis on health-related quality of life. Disabil Rehabil. 2003;25:1261–1303.
4. Mitchella J, Benito-León J, González JM, Rivera-Navarro J. Quality of life and its assessment in multiple sclerosis: integrating physical and psychological components of well-being. Lancet Neurol. 2005;4:556–566.
5. Al-Tahan AM, Al-Jumah MA, Bohlega SM. The importance of quality-of-life assessment in the management of patients with multiple sclerosis: recommendations from the Middle East MS Advisory Group. Neurosciences (Riyadh) 2011;16:109–113.
6. Benedict RH, Wahlig E, Bakshi R. Predicting quality of life in multiple sclerosis: accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. J Neurol Sci. 2005;231:29–34.
7. Lobentanz I, Asenbaum S, Vass K. Factors influencing quality of life in multiple sclerosis patients: disability, depressive mood, fatigue and sleep quality. Acta Neurol Scand. 2004;110:6–13.
8. Amato MP, Ponziani G, Rossi F, Liedl CL, Stefanile C, Rossi L. Quality of life in multiple sclerosis: the impact of depression, fatigue and disability. Mult Scler. 2001;7:340–344.
9. Kaynak H, Altintash A, Kayanak D et al. Fatigue and sleep disturbance in multiple sclerosis. Eur J Neurol. 2006;13:1333–1339.
10. Merlino G, Fratticci L, Lenchig C et al. Prevalence of “poor sleep” among patients with multiple sclerosis: an independent predictor of mental and physical status. Sleep Med. 2009;10:26–34.
11. Stanton BR, Barnes F, Silber E. Sleep and fatigue in multiple sclerosis. Mult Scler. 2006;12:481–486.
12. Fleming WE, Pollak CP. Sleep disorders in multiple sclerosis. Semin Neurol. 2005;25:64–68.
13. Manconi M, Ferini-Strambi L, Filippi M et al. Multicenter case-control study on restless legs syndrome in multiple sclerosis: the REMS study. Sleep. 2008;31:944–952.
14. Brass SD, Duquette P, Proulx-Therrien J, Auerbach S. Sleep disorders in patients with multiple sclerosis. Sleep Med Rev. 2010;14:121–129.
15. Kaminska M, Kimoff RJ, Benedetti A et al. Obstructive sleep apnea is associated with fatigue in multiple sclerosis. Mult Scler. 2012;18:1159–1169.
16. Beck SL, Schwartz AL, Towsley G, Dudley W, Barsevick A. Psychometric evaluation of the Pittsburgh Sleep Quality Index in cancer patients. J Pain Symptom Manage. 2004;27:140–148.
17. McCabe MP, Firth L, O'Connor E. A comparison of mood and quality of life among people with progressive neurological illnesses and their caregivers. J Clin Psychol Med Settings. 2009;16:355–362.
18. Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33:1444–1452.
19. Azimian M, Farahani AS, Dadkhah A et al. Fatigue severity scale: the psychometric properties of the Persian-version in patients with multiple sclerosis. Res J Bio Sci. 2009;4:974–977.
20. Krupp LB, Larocca NG, Muir Nash J, Steinberg AD. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–1123.
21. Vickrey BG, Hays RD, Harooni R, Myers LW, Ellison GW. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995;4:187–206.
22. Miller A, Dishon S. Health-related quality of life in multiple sclerosis: psychometric analysis of inventories. Mult Scler. 2005;11:450–458.
23. Ghaemi H, Borhan Haghighi A, Jafari P, Nikseresht AR. Validity and reliability of the Persian version of the multiple sclerosis quality of life questionnaire. Neurol India. 2007;55:369–375.
24. Kargarfard M, Eetemadifar M, Mehrabi M, Maghzi AH, Hayatbakhsh MR. Fatigue, depression, and health-related quality of life in patients with multiple sclerosis in Isfahan, Iran. Eur J Neurol. 2012;19:431–437.
25. Masoudi R, Mohammadi I, Nabavi SM, Ahmadi FA. The effect of Orem based self-care program on physical quality of life in multiple sclerosis patients. Shahrekord Univ Med Sci J. 2008;10:21–29.
26. Taraghi Z, Llali E, Abedini M et al. Quality of life among multiple sclerosis patients [in Persian] Iran J Nurs. 2007;20:51–59.
27. Haresabadi M, Karimi H, Forooghifar M, Mazloo SR. Quality of life among multiple sclerosis patients in Mashhad [in Persian] J N Khorasan Univ Med Sci. 2010;2:7–12.
28. Willoughby E. Modafinil for fatigue in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2002;72:150–155.
29. Solari A, Ferrari G. A longitudinal survey of self-assessed health trends in a community cohort of people with multiple sclerosis and their significant others. J Neurol Sci. 2006;243:13–20.
30. Benito-León NJ, Morales JM, Rivera-Navarro J. Health-related quality of life and its relationship to cognitive and emotional functioning in multiple sclerosis patients. Eur J Neurol Neurosurg Psychiatry. 2002;9:497–502.
31. Ghaem H, Haghighi AB. The impact of disability, fatigue and sleep quality on the quality of life in multiple sclerosis. Ann Indian Acad Neurol. 2008;11:236–241.
32. Merghati-Khoei E, Qaderi K, Amini L, Korte JE. Sexual problems among women with multiple sclerosis. J Neurol Sci. 2013;331:81–85.
33. Ayatollahi P, Nafissi S, Eshraghian MR, Kaviani H, Tarazi A. Impact of depression and disability on quality of life in Iranian patients with multiple sclerosis. Mult Scler. 2007;13:275–277.
34. Janardhan V, Bakshi R. Quality of life in patients with multiple sclerosis: the impact of fatigue and depression. J Neurol Sci. 2002;205:51–58.
35. Pajevic S, Basser PJ, Fields FD. Role of myelin plasticity in oscillations and synchrony of neuronal activity. Neuroscience. 2014;276:135–147.
36. Szilasiova J, Krokavcova M, Gdovinova Z, Rosenberger J, Van Dijk J. Quality of life in patients with multiple sclerosis in Eastern Slovakia. Disabil Rehabil. 2011;33:1587–1593.
37. Salehpoor G, Rezaei S, Hosseininezhad M. Quality of life in multiple sclerosis (MS) and role of fatigue, depression, anxiety, and stress: a bicenter study from north of Iran. Iran J Nurs Midwif Res. 2014;19:593–599.
38. Turpin KV, Carroll LJ, Cassidy JD, Hader WJ. Deterioration in the health-related quality of life of persons with multiple sclerosis: the possible warning signs. Mult Scler. 2007;13:1038–1045.
39. Fernández-Muñoz J, Moron-Verdasco A, Cigaran Mendez M et al. Disability, quality of life, personality, cognitive and psychological variables associated with fatigue in patients with multiple sclerosis. Acta Neurol Scand. 2015;132:118–124.
40. Kwiatkowski A, Marissal JP, Pouyfaucon M, Vermersch P, Hautecoeur P, Dervaux B. Social participation in patients with multiple sclerosis: correlations between disability and economic burden. BMC Neurol. 2014;14:115.
41. Huang L, Wang H, Li X. Study on the relationship between self-efficacy for disease management and quality of life among people living with HIV/AIDS. J Med Theory Pract. 2012;22:16.
42. D'Amico S, Marano A, Geraci MA, Legge E. Perceived self-efficacy and coping styles related to stressful critical life events. PloS One. 2013;8:e67571.
43. Kaminska M, Kimoff RJ, Schwartzman K, Torjan DA. Sleep disorders and fatigue in multiple sclerosis: evidence for association and interaction. J Neurol Sci. 2011;302:7–13.
44. Chervin RD. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest. 2000;118:372–379.
45. Hossain JL, Ahmad P, Reinish LW, Kayumov L, Hossain NK, Shapiro CM. Subjective fatigue and subjective sleepiness: two independent consequences of sleep disorders? J Sleep Res. 2005;14:245–253.
46. Karatepe AG, Kaya T, Guayaydin R, Demirhan A, Ce P, Gedizlioglu M. Quality of life in patients with multiple sclerosis: the impact of depression, fatigue, and disability. Int J Rehabil Res. 2011;34:290–298.
47. Buhse M, Banker WM, Clement LM. Factors associated with health-related quality of life among older people with multiple sclerosis. Int J MS Care. 2014;16:10–19.
48. Krokavcova M, Van Dijk JP, Nagyova I. Social support as a predictor of perceived health status in patients with multiple sclerosis. Patient Educ Couns. 2008;73:159–165.
49. DiLorenzo TA, Halper J, Picone MA. Quality of life in MS: does aging enhance perceptions of mental health? Disabil Rehabil. 2009;31:1424–1431.
50. Fischer JS, Prore RL, Jacobs LD. Neuropsychological effects of interferon beta-1a in relapsing multiple sclerosis. Ann Neurol. 2000;48:885–892.


