Perceived Impact of a Self-Management Program for Fatigue in Multiple Sclerosis
Why is this important to me?
Between 55 and 90% of individuals with MS experience fatigue. Many people with MS find that fatigue is one of the most difficult symptoms to manage. Fatigue interferes with patients' ability to care for themselves and their family, participate in daily activities, hold a job, and, in many instances, cope with other symptoms of MS. Management of MS-related fatigue is one of most important aspects of living well with MS.
What is the objective of this study?
People with MS participated in a six-week group program designed to help participants learn how to self-manage their MS-related fatigue. Telephone interviews were conducted with participants one and three months after completing the program to determine how well it helped them manage their fatigue. Two main themes related to perceived benefits of the program emerged from talking to participants:
- Participants changed their behavior to manage fatigue:
- Participants reported learning from other participants and learning through self-reflection.
- Participants reported that they learned how to take control of their fatigue by learning to accept their limits, set boundaries, select priorities, and take action. Participants learned to talk to other about their fatigue.
- Participants developed new habits to improve fatigue such as changing their mental approach, making time for rest, exercising, improving their nutrition, and becoming more organized.
- The effects of the program went beyond fatigue management and were useful in other aspects of their life:
- Participants developed a more resilient outlook toward fatigue, no longer felt alone, and learned to take control of their lives.
- Participants developed a new support network as they continued to meet with other participants after the program ended.
- Participants learned balance in their lives, believed that they were coping better, and learned to focus on the positives in their lives.
- Participants reported that they had better family dynamics because their family members had become more responsive to their needs. In addition, better management of participants’ fatigue allowed them to spend more time with their family members.
Overall, this program allowed participants to learn how to better self-manage their MS-related fatigue, which in turn improved many other aspects of their lives. Previous skills for managing fatigue were validated, and new skills were learned for problem-solving, decision-making, and taking action to manage fatigue. The benefits of the program lasted at least three months beyond its completion. The program provided participants with a feeling of personal accomplishment and improved their confidence as parents, partners, workers, and participants in the community.
How did the authors study this issue?
A six-week, group-based program designed to help people with MS self-manage their fatigue was developed by people with MS and was delivered to people with MS in New Zealand. The program included group meetings and the use of a workbook. Topics covered included the types of fatigue (mental, physical, emotional), physical activity/exercise, and achieving a home/work balance by planning and prioritizing goals. Participants (23 women with MS ranging in age from 37 to 63 years) were interviewed by phone one and three months after completing the program to determine if the program was beneficial and if new strategies learned were still working.
| SHARE: | |||||
Original Article
Perceived Impact of a Self-Management Program for Fatigue in Multiple Sclerosis A Qualitative Study
International Journal of MS Care
Hilda Mulligan, PhD; Amanda Wilkinson, PhD; Jessie Snowdon, BPhty, PGCertClinRehab
Background: Fatigue in multiple sclerosis (MS) is reported to be one of its most debilitating symptoms, affecting personal, family, and community participation. Despite a high incidence of MS in New Zealand, there was no cohesive approach to support people with MS to manage their fatigue. This prompted the development of Minimise Fatigue, Maximise Life: Creating Balance with Multiple Sclerosis (MFML), a group-based, 6-week fatigue self-management program. This study explored the perceived impact of MFML for participants who attended the program.
Methods: We undertook semistructured individual telephone interviews 1 (n = 23) and 3 (n = 11) months after delivery of the program. Data were analyzed for themes.
Results: Two themes emerged from the data: achieving behavior change to manage fatigue and whole of life effects. These themes represent participants’ perceived benefits of the program.
Conclusions: This study provides evidence that the MFML fatigue self-management program positively affected the lives of participants. The findings suggest that participants had begun to successfully develop and integrate self-management skills into their everyday lives. This affected the individual personally and also their participation in family and community life. This study adds to the current knowledge and understanding of the positive effect that delivery of a fatigue self-management intervention can have for people with MS.
The prevalence of multiple sclerosis (MS) is highest in countries that lie far north (eg, Scandinavia and the United Kingdom) and far south (eg, New Zealand). The prevalence of MS in New Zealand in 2010 was 71.3 per 100,000.1 Of all the symptoms that affect people with MS, fatigue has been shown to be correlated with higher levels of disability, depression, and interference with usual activities (eg, self-care, child care, work, and community engagement).2 MS-related fatigue has a reported prevalence of 55% to 90%,3 with many people reporting it as one of their worst symptoms.4 MS-related fatigue is described by those living with MS as unique, unpredictable, and misunderstood by others as to its effect on daily life and work. Fatigue intensifies other symptoms of MS, such as difficulty with walking, incontinence, spasticity, pain, visual deficits, and lack of concentration.5 Fatigue, therefore, makes everyday life more challenging.
A framework to improve health care for individuals with long-term conditions, such as MS, is Innovative Care for Chronic Conditions.6,7 This framework includes collaboration between health-care professionals and individuals living with long-term conditions in order to improve their self-reliance and confidence in self-managing their day-to-day symptoms and to maintain participation in usual and desired activities.8
Despite the high incidence of MS in New Zealand, there was no cohesive approach in the health service to help people with MS manage their fatigue. In addition, although studies investigating programs to address fatigue in MS have been reported in the international literature,9-13 the programs were not accessible to people living with MS in New Zealand. These issues prompted the development of Minimise Fatigue, Maximise Life: Creating Balance with Multiple Sclerosis (MFML), a group-based, 6-week self-management fatigue program and workbook now copyrighted to the Multiple Sclerosis and Parkinson’s Society Canterbury Inc.14 This program was designed to empower individuals with MS to develop self-confidence in managing their own symptoms of fatigue while learning together in a group situation. It is based on the self-management principles of problem solving, resource utilization, formation of partnership with the health-care provider and others with whom one identifies, decision making and taking action, and self-tailoring.15 Five health professionals from across New Zealand (New Zealand–registered physiotherapists and occupational therapists with experience working with people with MS in community settings) were trained in 2013 to deliver the program. Training consisted of an intensive 2-day face-to-face course (provided by JS) that explained the principles of self-management, role modeled delivery of the program, and included training for working with groups.
The program has been delivered twice (2013 and 2014) in five locations in New Zealand, with evaluation of the feasibility and efficacy of the program being undertaken during the second delivery.
Methods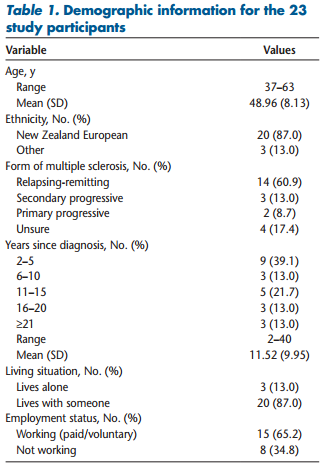
This study formed part of a mixed-methods evaluation of the MFML fatigue self-management program. Program evaluation was undertaken via self-report questionnaires and telephone interviews. This approach was chosen to increase the comprehensiveness of findings toward understanding the impact of MFML on the daily lives of individuals living with MS.16-18 This article reports findings from the telephone interviews. Ethical approval for the study was granted by the relevant University of Otago ethics committee (Dunedin, New Zealand).
Each of the health professional facilitators recruited a convenience sample of four to six individuals with MS to attend the program. Each attendee received a workbook that is divided into weekly sections. Each section provides information about a topic relevant to MS fatigue management (eg, types of fatigue, physical activity, and planning, prioritizing, and delegating for home- and work-life balance). The topics are accompanied by photographs of and quotes from the people with MS who participated in development of the program.14 Attendees also have the opportunity for written self-reflection and group reflection and discussion, with printed forms for writing action plans provided in the workbook.
Attendees were invited to take part in the study and, if they agreed, provided written informed consent to be part of this research. Individuals were included if they were older than 18 years with MS of any type or stage, able to communicate in English, and able to attend the program independently. Advertisement of the program was via information in each health professional’s health service(s), in MS Society newsletters or local general practices, or via outreach personnel of MS societies. A total of 26 individuals with MS attended the program, and 23 agreed to be interviewed for this study. All the participants were women, with an age range of 37 to 63 years. Table 1 provides further demographic information.
Data Collection
Two semistructured individual telephone interviews were used to gather data. These interviews occurred approximately 1 and 3 months after the end of the program. We contacted each participant via e-mail to arrange a suitable time to conduct a telephone interview. Two members of the research team (HM, AW) conducted the interviews using open-ended questions that explored 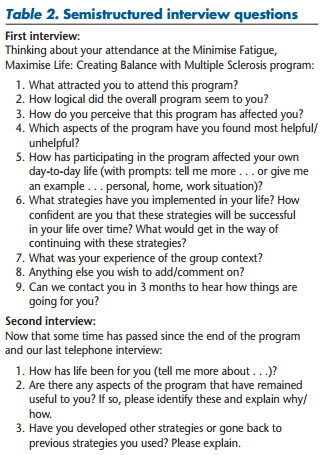 participants’ perceptions of the impact of the program on their lives (Table 2). The first interviews (with 23 participants) took approximately 20 to 30 minutes, and the second interviews (with 11 participants) were 10 to 15 minutes long. In this follow-up interview, we asked participants how life was for them, and we explored the ongoing benefits of the program to them (ie, whether strategies they had reported on in the first interview were still working and whether they had added to or changed these). Interviews were audiotaped and then transcribed verbatim by the researchers who had conducted the interviews. Personal identification information was then removed, and the transcripts were numbered to maintain participant anonymity.
participants’ perceptions of the impact of the program on their lives (Table 2). The first interviews (with 23 participants) took approximately 20 to 30 minutes, and the second interviews (with 11 participants) were 10 to 15 minutes long. In this follow-up interview, we asked participants how life was for them, and we explored the ongoing benefits of the program to them (ie, whether strategies they had reported on in the first interview were still working and whether they had added to or changed these). Interviews were audiotaped and then transcribed verbatim by the researchers who had conducted the interviews. Personal identification information was then removed, and the transcripts were numbered to maintain participant anonymity.
Data Analysis
We analyzed the data thematically using an inductive approach.19 To do this, two members of the team (HM, AW) worked together with the first interview transcript to develop an initial coding template that identified sections of the text that pertained to benefits of the program to the participant. Each code was given a description and then was tabulated to create a coding template. This coding template was then used to analyze the remaining transcripts. The two researchers coded these independently, adding new categories as they emerged, and discussing these before adding them to the template. Data saturation was reached after interview 17. However, we did continue to analyze all of the data. The whole team then met together over a 6-week time frame to synthesize the categories into themes.
Results
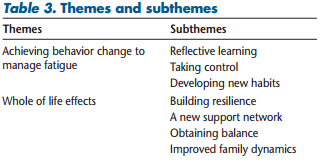
Two themes emerged from the analysis: 1) achieving behavior change to manage fatigue and 2) whole of life effects. Both themes represent perceived benefits of the program for participants. The themes are described herein, including their subthemes (Table 3) and supporting quotes taken from transcripts. The quotes have been identified, for example, as participant 1:1 (for participant 1, interview 1) or participant 1:2 (participant 1, interview 2).
Theme 1: Achieving Behavior Change to Manage Fatigue
This theme showed the processes that resulted in achievement of new behaviors by participants toward improved management of their fatigue. The theme was derived from the subthemes of 1) reflective learning, 2) taking control, and 3) developing new habits.
The reflective learning subtheme comprised categories pertaining to new learning (imparted via the program’s content and facilitator), learning with and from other attendees, and learning through self-reflection, which included identification of new strategies and discovery and validation of already used strategies: “I didn’t realize there were things like mental and emotional fatigue as well as physical [fatigue]” (participant 12:1). “Input from fellow attendees was also a gem because between the five [attendees], the total number of years we had the illness was 103—that’s a lot of experience” (participant 13:1). “What was most helpful was stopping to think and identifying which things were the hardest and most draining for me and thinking up ideas for how I could make it easier” (participant 8:1).
 The taking control subtheme reflected how participants had learned to accept their limits, set boundaries, decide on priorities, and then work out what to do and do that as a priority: “I used to get up at 7 a.m. and have a shower straight away and I’d start the day off completely wiped out . . . and you kind of feel sad because you feel so tired. Whereas now I wait until the kids are off to school. I start the day off feeling happy and positive and it’s just, it’s incredible how something so little can make such a huge, huge difference” (participant 9:2). “I write myself a weekly plan, list things down that I want to achieve and then I put them into a time schedule for myself and I’m really open and I discuss it with my husband” (participant 15:1).
The taking control subtheme reflected how participants had learned to accept their limits, set boundaries, decide on priorities, and then work out what to do and do that as a priority: “I used to get up at 7 a.m. and have a shower straight away and I’d start the day off completely wiped out . . . and you kind of feel sad because you feel so tired. Whereas now I wait until the kids are off to school. I start the day off feeling happy and positive and it’s just, it’s incredible how something so little can make such a huge, huge difference” (participant 9:2). “I write myself a weekly plan, list things down that I want to achieve and then I put them into a time schedule for myself and I’m really open and I discuss it with my husband” (participant 15:1).
Furthermore, participants had learned to prioritize, partly through improved communication with their family but also via communicating the effects of MS on their life to others. For example, one participant related how she had gained the courage to explain the debilitating and fluctuating fatigue of MS to her child’s schoolteacher. This had allowed the teacher to understand why the participant had not volunteered to participate in a school outing because she considered her fatigue a potential safety issue.
In the developing new habits subtheme, participants reflected on how they had developed new habits to improve daily life. In this example, a participant identified changing her mental approach to living with fatigue: “We’re going away for a week in the school holidays and I was really concerned about it and that I was going to be too tired. So I was thinking maybe I shouldn’t go because I wouldn’t be able to do any of the things I wanted to do with the kids. And they [other attendees] said to me, ‘Well, it sounds like you’re trying to talk yourself out of it.’ I thought, ‘Oh, it does sound like that, doesn’t it?’ So this really made me look at how I think about things. I think I have been setting up roadblocks before I even get there. So it’s been really good to look at the way I was thinking” (participant 7:1).
Participants also developed new habits around preventive or restorative rest: “One of my biggest downfalls is that in my busy [work] schedule I came to not put in time for rest. I know I have to do it and I will just do it when my body needs it. But that’s kind of waiting for your energy levels to drop, rather than planning and fitting in a rest before you go downhill” (participant 2:1).
Other new habits that were developed were the incorporation of exercise, personal nutrition, and better organization for family requirements into their schedules: “What I found incredibly positive is that you can work on your fitness, and you can increase your well-being through exercise, you know, despite everything else, as long as you do it cleverly. Exercise is much more a part of my life this year than it ever has been, which is just great” (participant 3:2).
Theme 2: Whole of Life Effects
The second theme identified that the overall effect of the program extended beyond fatigue management to many other facets of life for participants. The theme included the subthemes of 1) building resilience, 2) a new support network, 3) obtaining balance, and 4) improved family dynamics.
The building resilience subtheme showed how the opportunity to reflect with others living with MS became a learning experience toward building resilience. For some participants this was because they no longer felt alone since meeting other people with MS who also experienced fatigue: “This is something I have not had in the past and it has been a long and lonely journey for me. Now my life is brighter, my spirits raised, and I have the purpose and contentment I mentioned earlier. Thanks to all of you for your invaluable input, it is so much appreciated” (participant 19:2). “It’s been an absolute godsend because just realizing you’re not the only person that suffers from this has been great for me” (participant 16:1).
Alternatively, other participants were emotionally confronted by experiencing MS en masse because this had highlighted the potential impact of MS on their life in the future: “Our stages for where we are with MS were too different, and I felt drained and saddened. You don’t want to hear all the stories and symptoms they have and compare who had it worse. [But] I also found that I am a lot stronger than what I thought, and I thank [attendance at the program] for that” (participant 1:1). Whichever side of the coin their experience came from, participants had learned through this that they needed to take control of their own situation, and they used the opportunity of attendance at the program to do so.
Many participants mentioned meeting up with other attendees on a semiregular basis after the end of the program. This encapsulated the new support network subtheme. This had boosted participants’ morale and will, if it continues, provide them with an informal support network: “We’re going to catch up. We’re going to keep in touch” (participant 15:1). . . . “Met with group for lunch twice and it was beneficial” (participant 15:2).
The obtaining balance subtheme showed how participants perceived themselves to be coping well with new strategies in day-to-day life and also how they now could look for the positives in their lives: “I look for positives, even little positives” (participant 13:1). “And it’s really nice to have something [exercising] that [makes you feel] like a normal person [laughs]. You might have a plan or an aim or a goal and you too can be part of that sort of going forward sort of thinking” (participant 3:1).
The improved family dynamics subtheme captured how participants perceived that they had a more responsive family or spouse as a result of attending the program: “I will say to my parents, ‘Oh, I’ve been really fatigued today,’ and Mum will go, ‘Oh, you’ve been overdoing it?’ And I’ll go, ‘Yeah.’ But before if I said, ‘I’ve been feeling really tired today,’ they’d say, ‘Oh well, you should’ve gone to bed earlier.’ So [communicating clearly] does put a different spin on it” (participant 7:1). They reported how better management of fatigue resulted in their having more energy and, therefore, more time to spend with the family. This had been noticed and acknowledged by the family as being enjoyable: “He’s obviously noticed that we have more family time now, like, he came out of the blue saying let’s go to [previously enjoyed recreation area]. In the past I wouldn’t be able to, I would be too tired; whereas now at the weekend, we have [lots of] family time, which is really good” (participant 9:1).
Discussion
The purpose of this study was to explore the perceived impact of the MFML fatigue self-management program from the participants’ perspective. The themes of achieving behavior change to manage fatigue and whole of life effects suggest that participants had begun to successfully develop and integrate the self-management skills of problem solving, decision making, taking action, and self-tailoring15 for managing fatigue in their daily lives. Self-management is much more than the ability to follow a prescribed treatment plan; it encompasses the use of personal knowledge and awareness of how the body responds to internal and external stimuli to maintain balance in life.20-22 This is important because it is the individual who lives with the need to independently manage their condition on a daily basis.23 In the present study, self-management skill development was facilitated in the program through education about what fatigue is (both physical and mental) and through personal understanding of the effect of fatigue on daily living and vice versa, that is, that daily living had an effect on levels of fatigue. This increased awareness enabled the individuals to be receptive to the content of the program and to appreciate the need to make changes in their life to better manage fatigue.
In addition, MFML supported the participants’ development of self-efficacy24,25 through affirmation or validation of previous strategies used to manage fatigue or by identification and attainment of new fatigue management strategies. Together with the perceived reliability of the source of the new information (via the program’s workbook and listening to others’ experiences), these provided a feeling of personal accomplishment. Development of self-management and self-efficacy skills aims to provide individuals with the confidence to cope and deal with the emotional and medical impact of the disease on their lives26 and to improve confidence for their life roles (such as parenting, partnering, and working).24,25 The MFML was developed by people with MS for people with MS. This gives credibility to the program because it reinforces the self-efficacy principles of learning from others with whom one can identify.24,25
Development of the MFML program was first presented at a New Zealand physiotherapy conference. As a result of physiotherapists spreading the word about the program to occupational therapy colleagues, the first trainees to deliver the program were occupational therapists or physiotherapists. Future training could include other health professionals, with nurses and social workers having already expressed interest.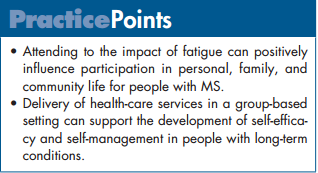
Although studies have demonstrated the efficacy of fatigue management for people with MS,10-13,27 with reductions in the impact of fatigue and improvements in self-efficacy and quality of life, there is limited research exploring the impact of fatigue management programs on people’s lives from their own perspectives. A qualitative approach provides personal insight into the potential impact of a program on individuals’ lives. The present findings build on a similar study using interviews and group sessions with seven participants.28 Hence, the present study adds to the knowledge and understanding of the effect of fatigue management programs for people with MS.
One limitation of this study was that all the participants were women and, therefore, the findings may not be similar for men living with MS. Although the first set of interviews occurred early after the end of the program (when attendees may not have yet consolidated learning for fatigue self-management), the 3-month interviews provided evidence that participants had maintained and even increased benefit from the program. Another limitation was that although all 23 participants agreed to a follow-up interview, only 11 of the 23 responded positively to the e-mail request to schedule a time for the second interview to occur. Therefore, maintenance and increased benefit from the program over time may apply to only approximately half of the attendees at such a program.
Conclusion
This study provides evidence that the MFML fatigue self-management program positively affected the lives of participants. The findings suggest that participants had begun to successfully develop and integrate the selfmanagement skills of problem solving, decision making, taking action, and self-tailoring for managing fatigue in their daily lives. This had a personal impact not only on their daily coping mechanisms and perceived impact of fatigue but also on their participation in family and community life. The findings from this study add to the depth of understanding about fatigue management for people with MS. Evidence of efficacy for this program provides health professionals and people with MS in New Zealand with an accessible program for fatigue management. In addition, the program has the potential for further development for people with other chronic health conditions.
Acknowledgements: We thank the participants for their contributions and willingness to take part in this study. We also thank the health professional facilitators who delivered the program for their interest in and support of this study.
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This study was supported by a University of Otago research grant to Dr. Mulligan.
REFERENCES:
1. Taylor BV, Pearson JF, Clarke G, et al. MS prevalence in New Zealand, an ethnically and latitudinally diverse country. Mult Scler. 2010;16:1422–1431.
2. Pittion-Vouyovitch S, Debouverie M, Guillemin F, Vandenberghe N, Anxionnat R, Vespignani H. Fatigue in multiple sclerosis is related to disability, depression and quality of life. J Neurol Sci. 2006;243: 39–45.
3. Tellez N, Rio J, Tintore M, Nos C, Galan I, Montalban X. Fatigue in multiple sclerosis persists over time: a longitudinal study. J Neurol. 2006;253:1466–1470.
4. Smith C, Hale L. The effects of non-pharmacological interventions on fatigue in four chronic illness conditions: a critical review. Phys Ther Rev. 2007;12:324–334.
5. MacAllister WS, Krupp LB. Multiple sclerosis-related fatigue. Phys Med Rehabil Clin N Am. 2005;16:483–502.
6. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient selfmanagement of chronic disease in primary care. JAMA. 2002;288: 2469–2475.
7. World Health Organization. Innovative Care for Chronic Conditions: Building Blocks for Action. http://www.who.int/chp/knowledge/publications/icccglobalreport.pdf?ua=1. Accessed December 17, 2015.
8. Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364:1523–1537.
9. Finlayson M, Plow M, Preissner KL, Cho C. Randomized trial of a teleconference-delivered fatigue management program for people with multiple sclerosis. Mult Scler. 2011;17:1130–1140.
10. Mathiowetz V, Finlayson ML, Matuska KM, Chen HY, Luo P. Randomized controlled trial of an energy conservation course for persons with multiple sclerosis. Mult Scler J. 2005;11:592–601.
11. Mathiowetz V, Matuska KM, Murphy ME. Efficacy of an energy conservation course for persons with multiple sclerosis. Arch Phys Med Rehabil. 2001;82:449–456.
12. Moss-Morris R, McCrone P, Yardley L, van Kessel K, Wills G, Dennison L. A pilot randomised controlled trial of an Internet-based cognitive behavioural therapy self-management programme (MS Invigor8) for multiple sclerosis fatigue. Behav Res Ther. 2012;50:415–421.
13. Finlayson M. Pilot study of an energy conservation education program delivered by telephone conference call to people with multiple sclerosis. NeuroRehabilitation. 2005;20:266–277.
14. Mulligan H, Wilkinson A, Lusty A, Delorme A, Bong S. Consumers and health professionals’ perceptions of Participatory Action Research in developing a health resource. N Z J Physiother. 2015;43:93–97.
15. Lorig K, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7.
16. Greene J. Mixed Methods in Social Inquiry. San Francisco, CA: JosseyBass; 2007.
17. Greene J, Benjamin L, Goodyear L. The merits of mixing methods in evaluation. Evaluation. 2001;7:25–44.
18. Greene J, Caracelli V, Graham W. Toward a conceptual framework for mixed-method evaluation designs. Educ Eval Policy Analysis. 1989;11:255–274.
19. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
20. Rogers A, Kennedy A, Nelson E, Robinson A. Uncovering the limits of patient-centeredness: implementing a self-management trial for chronic illness. Qual Health Res. 2005;15:224–239.
21. Paterson B. The shifting perspectives model of chronic illness. J Nurs Scholarship. 2001;33:21–26.
22. Paterson B. The koala has claws: applications of the shifting perspectives model in research of chronic illness. Qualitat Health Res. 2003;13:987–994.
23. Wilson P, Mayor V. Long-term conditions, 2: supporting and enabling self-care. Br J Commun Nurs. 2006;11:6–10.
24. Bandura A. The explanatory and predictive scope of self-efficacy theory. J Soc Clin Psychol. 1986;4:359–373.
25. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215.
26. Adams K, Greiner A, Corrigan J, eds. Report of a Summit: The 1st Annual Crossing the Quality Chasm Summit–A Focus on Communities. Washington, DC: National Academies Press; 2004.
27. Vanage SM, Gilberston KK, Mathiowetz V. Effects of an energy conservation course on fatigue impact for persons with progressive multiple sclerosis. Am J Occup Ther. 2003;57:315–323.
28. Preissner KL. “A Group of Me’s”: Adult Learning Through Group Process: The Experiences of Participants in a Teleconference Delivered Multiple Sclerosis Fatigue Management Program [dissertation]. Dekalb: Northern Illinois University; 2013.
