Home Modification
Why is this important to me?
If you have lived with MS for many years, you may be experiencing disability or limitations. You may experience gait and balance problems that make you more likely to fall, or you may require the use of assistive devices such as a cane or wheelchair. Your home may not be configured to accommodate these limitations and devices. Modification of your home may decrease your likelihood of falling and increase your independence and quality of life.
What is the objective of this study?
Most homes contain some hazards that may increase your chance of falling or may lower your independence if you have certain physical limitations. Although relocation to an assisted-living facility is an option for some people, many people prefer to live in their own homes. Home modifications may be a good alternative to people wishing to stay in their own homes.
A few studies have examined the effectiveness of home modification for prevention of falls. Behavioral changes such as strength and balance training can also help prevent falls. Overall, studies looking at home modification and/or behavioral changes show that falls can be reduced by about one-third with certain interventions, especially in people with a history of falling. Interventions and modifications may also help reduce the medical costs associated with a fall.
To determine which interventions will be most beneficial to you, think about which assistive devices you use and what daily activities are most challenging for you (climbing stairs, bathing, using the bathroom, moving throughout the house, cooking, etc.).
Some modifications that can be made quickly, easily, and with little or no expense include:
- Install grab bars in the bathroom
- Use non-skid bath mats
- Use a raised toilet seat
- Remove loose rugs and other loose items that you could trip on
- Place furniture so that chairs, sofas, etc. that can help you balance are accessible and that furniture that you may trip on is out of your way
- Use remote controls for various appliances
- Place Lazy Susans and pull-out shelves throughout your house
- Installing lever or loop handles rather than knobs for doors, cabinet drawers, and faucets
Other modifications may be more extensive or expensive such as:
- Install a roll-in shower that allows a wheelchair to enter
- Install a built-in seat in the shower stall
- Install a moveable, hand-held showerhead on a flexible hose to permit showering while seated
- Install special hinges on your doors that let the doors open wider to better accommodate a wheelchair
- Modify thresholds so that they are as low as possible
- Purchase chairs with arms or a lift chair that can be used to help you stand from a seated position
- Create open, clear space under counters and sinks (helpful if you use a wheelchair or work while seated)
- Purchase a side-by-side refrigerator
- Install stairs with short risers and handrails
- Replace a swinging door with a pocket door
- Purchase washers and dryers with front-mounted controls
- Install a ramp with handrails so that you do not have to use stairs to enter a house
Remember, many of these modifications provide convenience and safety to most people, not just individuals with disability. Also, many of these modifications will make your home more comfortable for yourself as well as for visitors you may have with disabilities or limitations.
How did the author study this issue?
The author reviewed current strategies for people with disabilities, limitations, or a likelihood to fall for modification of their homes to increase their safety and independence. This article is not specifically about people with MS, but rather is written for anyone living with a disability.
| SHARE: | |||||
Original Article
Home Modification
American Journal of Nursing
Marjorie Cook McCullagh, PhD, RN,BC, COHN-S
Overview: Almost 50 million Americans—about one in five—live with a mental or physical disability, many in homes that are inconvenient, restrictive, or dangerous for them. Modifying the home using universal (barrier-free) design, architectural accessibility, and other such concepts can reduce the risk of falls and improve overall function. Nurses can be involved by assessing patients’ living quarters and recommending specific modifications.
Ellen Thomas, a 50-year-old retail manager, lives alone in a two-story duplex. Her mother, Eveline Crane, age 70, has lived for many years in a one story ranch house about an hour’s drive away. Ms. Crane was recently widowed and likes living alone, but she’s becoming increasingly frail. Ms. Thomas has considered asking her mother to move in with her but is hesitant, believing her home isn’t well suited to this arrangement: for example, the spare bedroom is on the second floor.
Jerry and Mary Hartford, both high school teachers, live in a small apartment with their six-year-old son, Max, who has cerebral palsy and uses a wheelchair. They are planning a new house and are wondering how to modify its design in order to accommodate the larger wheelchair he is expected to use as he grows.
These cases, composites based on the author’s experience, illustrate two of the many situations in which suitability of housing can be an issue. According to the U.S. Census Bureau, almost 50 million Americans five years of age and older (19% of the total population) live with a mental or physical disability.1 Of these, an estimated 25 million have difficulty walking and 18 million have difficulty “lifting and carrying a 10-pound bag of groceries or grasping small objects.”1 About one-third of all those with disabilities are ages 65 or older (14 million), while two-thirds are younger, including about 31 million adults ages 21 through 64 and 5 million young people ages five through 20.1 Nurses have been assisting patients in making their homes safer and more accessible for decades, but new concepts in home modification may help to further improve patients’ lives.
NEITHER SAFE NOR SUITABLE
Many people live in homes that are ill-suited to their needs. Pynoos and Sanford succinctly describe such residences as “‘Peter Pan Housing,’ designed for people who never age.”2 Nor is aging the only consideration; disability can occur at any time of life (indeed, some activists seeking to raise awareness sometimes refer to those who are not disabled as “temporarily able-bodied.”3 ) Many people find themselves living in homes with features that at one time were acceptable but are now inconvenient, restrictive, or dangerous, such as stairs that must be climbed or appliances that require bending.
In a study of fall-prevention strategies in the homes of 252 Australian older adults (mean age, 69 years), fall hazards such as the absence of grab bars in the bathroom or unsecured mats on the floor were present in nearly all homes studied, with an average of 10 hazards per home.4 In another study focusing on fall prevention in the elderly, an occupational therapist visited 178 homes and recommended at least one modification in 150 of them (84%).5 Recommendations included removing mats and throw rugs, rerouting electrical cords, and installing stair and bath rails.
Aging in place. Although a recent review concluded that the rate of disability among older Americans is declining, it is still high: the review reported that one in five older Americans has a chronic disability and one in three has limited mobility.6 For some people, one solution to an unsuitable home is relocation to a retirement or assisted-living facility. Yet according to the AARP, more than 80% of adults ages 45 and older “strongly or somewhat agree that they would like to remain in their current residence for as long as possible” as they age—a concept often referred to as “aging in place.”7 The advantages of aging in place are many, including avoiding the high costs of institutional care and maintaining established connections within the community. Encourage patients, regardless of their age, to be mindful of the potential need for modifications whenever they make housing choices.
SMALL CHANGES, BIG IMPROVEMENTS
Two major concepts in the field of home modification are universal design (sometimes called barrier free design) and architectural accessibility. Universal design refers to creating new products and environments that can be “usable by all people, to the greatest extent possible, without the need for adaptation,” as well as to altering existing products and settings as needed.8 Architectural accessibility refers to constructing or remodeling a building so that its structure and design do not restrict access or use by people with disabilities.9, 10 Another concept that has gained notice is visitability, which refers to making all homes compliant with basic accessibility features (at least one entrance without steps, wider-than-standard doorways, and at least one half-bathroom on the first floor) so that people with impaired mobility can visit anyone easily, allowing them fuller “participation in the life of the community.”11, 12
Using these concepts, architects, rehabilitation engineers, and assistive technology specialists are designing new homes and modifying existing ones so that they are suitable for people with current disabilities as well as those whose disabilities have yet to emerge. By assessing patients’ living quarters and recommending specific modifications, nurses can help to reduce or eliminate home hazards, defer or eliminate costly alterations, and make the home usable by residents and visitors of varying abilities.
Some modifications, such as installing grab bars and removing loose rugs, can be made with little or no alteration to underlying structures; others, such as installing stairs with risers that are shorter than standard height, may involve major remodeling or are best planned before home construction begins.
THE BENEFITS OF CHANGE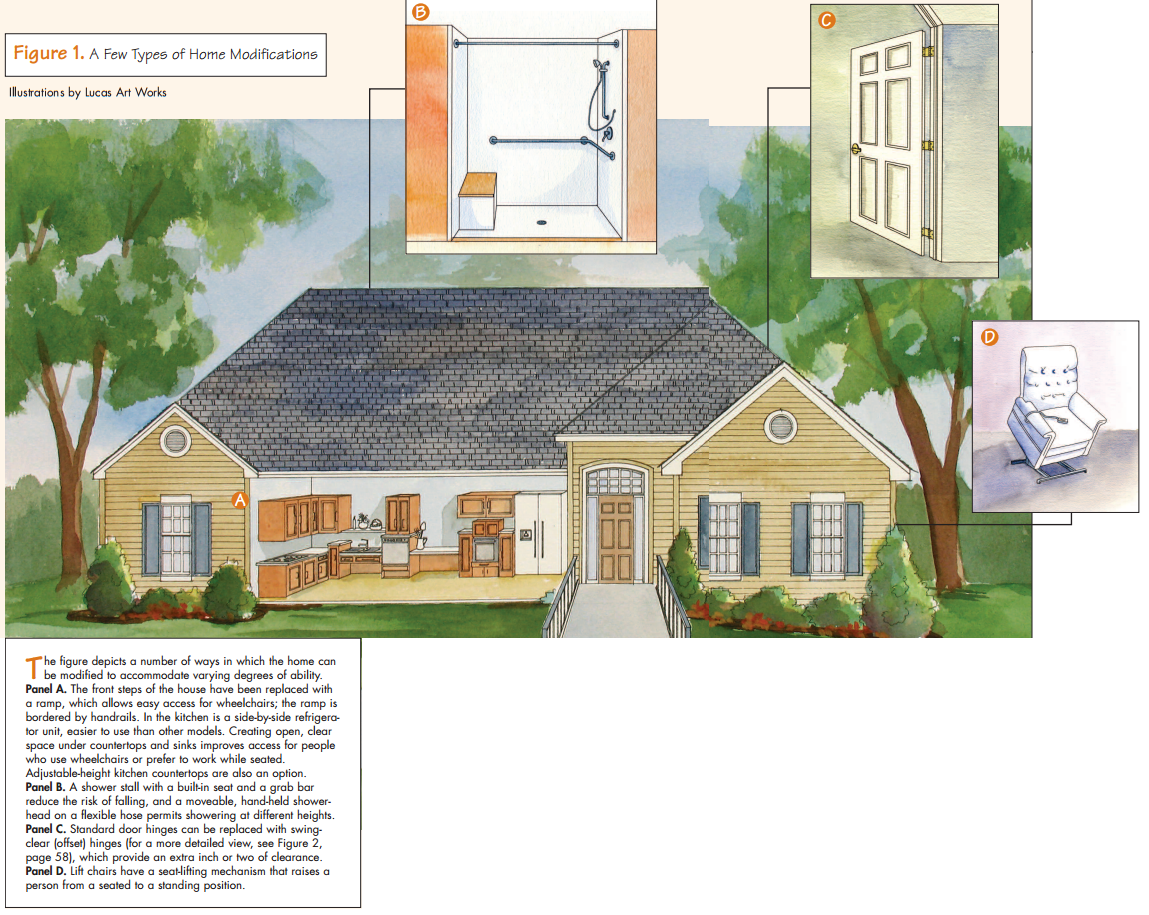
Several randomized, controlled studies have examined home modifications as part of a comprehensive intervention to prevent falls in the elderly. A review of the literature revealed no studies examining the effectiveness of home modifications alone (that is, without in-home assessment or patient education) or the effectiveness of specific home modifications (such as the installation of grab bars). Still, taken together, the results suggest that home modifications are a valuable component of strategies to prevent falls, particularly among people who have recently fallen. There are few studies examining the impact of home modifications on overall function; more research is needed.
Preventing falls. Tinetti and colleagues studied 301 enrollees in a health maintenance organization who were 70 years of age and older and had at least one risk factor for falling.13 These included impairment in one or more areas: arm or leg strength, range of motion, balance, gait, or ability to transfer from chair to bathtub or toilet (“transfer skills”). Participants were randomized into two groups: 153 received an intervention that included home assessment for fall hazards as well as exercises to improve balance, gait, and transfer skills, while 148 enrollees received “usual health care.”13 Patients with difficulty transferring also received appropriate modifications (including grab bars, nonskid mats, and elevated toilet seats). During the one-year follow-up, 35% of those in the intervention group fell and 47% of the controls did; the researchers acknowledged that it was impossible to know which interventions were responsible for the decrease. A study by Close and colleagues involving 304 older adults treated at an ED for injuries caused by falls showed comparable findings.14
In a study of 530 older adults, most of whom were recently discharged from a major teaching hospital, Cumming and colleagues looked specifically at the role of home modifications in reducing the rate of falls.15 An occupational therapist assessed the homes of the 264 patients in the intervention group for fall hazards, recommended modifications—the most common were removal of loose mats and throw rugs and the use of nonslip bath mats—and telephoned shortly afterward to encourage adherence. During the year of follow-up, the intervention reduced falls by 36% among those with a history of falls but had no significant effect in people with no history of falls. The researchers speculated that the intervention’s effectiveness may have resulted in part from suggested behavioral changes (not specified) and not from home modifications alone.
At least one other study illustrates the effectiveness of home modifications among people with a history of falls. Among 360 frail older adults who had fallen recently, Nikolaus and Bach evaluated an intervention that included home assessment for hazards, recommendations for and assistance with modifications, and training in using “technical and mobility aids.”16 The intervention group demonstrated 31% fewer falls than the control group.
Improving function. One study involving 171 home-dwelling people with dementia and their family caregivers evaluated an intervention that sought, in part through home modifications, to create an environment “supportive of reduced competencies”; its aims were to reduce the caregivers’ stress and to improve the patients’ function and behavior. 17 The researchers found that, according to the caregivers, patients in the intervention group retained significantly better function in independent activities of daily living (IADLs) than did those in the control group, and their caregivers’ burden was also somewhat lower. But there were no significant differences between the two groups in other activities of daily living (ADLs).
Based on an economics model, one study used a representative sample of 907 people age 70 years and older to examine how losses in the ability to bathe might be reversed.18 Kutty found that modifications such as grab bars and shower seats resulted in improvements, especially among those age 80 years and older. She concluded, “It is likely that other home modifications and equipment also have similar effects.” And in a randomized, controlled trial among 319 community-dwelling older people with functional difficulties, Gitlin and colleagues found that home modifications, combined with instruction in safety and balance and muscle-strength training, resulted in improvements in the performances of ADLs and IADLs after six and 12 months.19
The cost effectiveness of home modifications in preventing falls was the focus of Salkeld and colleagues’ randomized, controlled trial of 530 older adults, most of whom had recently been inpatients at a major teaching hospital (the same cohort studied in Cumming and colleagues15).20 The intervention, which featured home modifications, resulted in fewer falls but higher health care costs. The intervention “achieved [a median cost of] $2,853 per fall prevented for all subjects and just $119 per fall prevented for subjects with a history of falls.” The higher overall health costs were found to be unrelated to the intervention. The researchers concluded that the intervention was “cost saving amongst those people who had fallen in the year prior to recruitment.”
Other benefits. Even people without disabilities find certain features of their homes challenging. For example, most kitchen counters in this country are designed for use by a woman of average height (about 594021). Taller people may need to bend over to work, and children and shorter adults may have difficulty reaching.
Yet many people who might benefit from modifications to the home go without them.22-24
ASSESSING NEEDS AND ADDRESSING BARRIERS
Although there are no established standards for making home modifications, recommendations can be made on the basis of assessment. A visit to the patient’s home is the best method.
Some types of disabilities, including some that are congenital or those that result from injury, present an obvious need for home modification. Other disabilities, such as those associated with many chronic illnesses, develop more slowly and may be easier to ignore. Still others, such as hearing loss, may not be apparent or visible.
During assessment, consider the patient’s diagnoses and disabilities and which assistive devices he uses. Ask him to identify difficulties with ADLs (including bathing, dressing, eating, using the toilet, and transferring in and out of bed and chairs) and IADLs (including meal preparation and household chores such as laundry); keep in mind that each of these involves many small tasks. For example, brushing one’s teeth often entails entering a bathroom, switching on a light, opening a medicine cabinet, and turning on a faucet, in addition to preparing and using a toothbrush. Observing the patient in a variety of situations will give precise information about his challenges and abilities. As one review author commented, observation is preferred over the patient’s report “because patients often overestimate their functional ability.”25
Addressing barriers. Studies show that a majority of patients follow at least some of the recommendations for change.4, 5, 17 But some people have to make a psychological adjustment to the idea of modifying a home. They may be reluctant to alter a cherished or familiar home or fear the prospect of their own decline. In one study, respondents’ explanations for not making suggested home modifications included failing to see any reason to make changes (49%), perceiving the home environment as safe (34%), and believing oneself not to be at risk for falls (17%).5 Only 1% indicated they could not afford to make modifications.
One company has developed the Comprehensive Assessment and Solution Process for Aging Residents (CASPAR; available at www.ecaspar.com/ec/ caspar.pdf or by calling [847] 215-9490), which health care professionals can use in assessing homes and specifying modifications.26 Although CASPAR has been used for years, its validity and reliability have not been established scientifically. Using CASPAR, the health care worker first asks the patient whether he has difficulty with daily activities at home and discusses what changes he is willing to make and what he wants left unaltered, then takes measurements and photographs of the areas to be changed.
Patients and families who are initially reluctant to make suggested modifications may not be aware of the beliefs that underlie their opposition, such as the following26:
- My disability is temporary.
- Home modifications will make it obvious to visitors that I’m disabled.
- Home modifications are unattractive.
- Other people (such as family members, my landlord, and my neighbors) will disapprove.
- The modifications will be too costly.
Begin the conversation by gently asking the patient how he feels about these statements. Some people may be more willing to modify their homes if they believe that others living with them will also benefit.
Cost is a common concern. Many local governments offer assistance to qualified people for some items (such as grab bars and elevated toilet seats). Refer the patient to a local or state office for the elderly or people with disabilities to find out about free or reduced-cost services. The U.S. Department of Veterans Affairs offers grants for home modifications for eligible veterans; contact the local office of veterans’ affairs (www.va.gov/directory/guide/home.asp).
If the patient and family seem overwhelmed, they may need help identifying resources or finding skilled contractors. In addition to providing education, help the patient prepare a list of suggested changes for discussion with a professional installer or a friend with home-improvement skills. In many cases, family members, friends, and neighbors are able to assist with these tasks. You can also contact the local affiliate of the National Association of Home Builders (www.nahb.org).
STRATEGIES 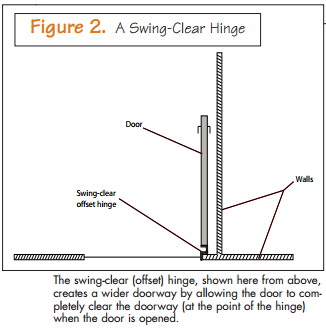
Some home modifications for a variety of common disabilities and limitations follow.
Impaired mobility or agility. When assessing for changes in mobility (the ability to move), agility (the ability to move with ease and quickness), or both, observe for difficulty in walking, climbing stairs, standing from a seated position, and moving easily and quickly. Difficulties in these areas are very common, particularly among older people. Ask the patient to demonstrate navigating stairs and pathways, carrying loads, reaching for low or high shelves, getting in and out of the tub or shower, and using the toilet. As he walks through the home, assess his ability to adjust his gait to different surfaces, as when crossing thresholds. Some patients will seek assistance intermittently, by grabbing onto nearby furniture for example, or touching or leaning against walls for stability. People who use wheelchairs are likely to have limitations in one or more of these areas.
Floors and doors. One way to improve access is to eliminate anything that obstructs movement across floors and through doorways. For example, most doorways in houses are too narrow for wheelchairs and may be restricting for people using walkers, crutches, or canes. Doors may not swing sufficiently out of the way. Several changes can address this27:
- Standard door hinges can be replaced with swing-clear (offset) hinges (see Figure 2), which permit the door to clear the opening space completely, providing an extra 1 or 2 in. AARP recommends that all doorways have clear openings that are at least 32 in. wide.28
- A swinging door can be replaced with a pocket door (a door that slides into a pocket created in a wall).
- A ramp or berm (an earthen ramp) can be installed to ease access to a building—not only for wheelchair use but also any wheeled devices such as hand carts, strollers, or rolling luggage. Of course, they can be used by anyone for whom stairs may be challenging, including toddlers. Constructing the ramp inside an attached garage eliminates the need to clear ice and snow from it during winter months.
For some, the transition from one type of floor surface to another (such as from vinyl flooring to carpet) is a challenge because the adjoining surfaces often differ in height. People with disabilities affecting mobility, such as gait disturbances, often find these differences in height or texture to be a tripping hazard or otherwise difficult to navigate.8 One solution may be to modify one of the floor surfaces; for example, plush carpeting can be replaced with a low-pile alternative.29 Area and throw rugs are notorious for causing falls; they should be removed or avoided whenever possible.29 If they must be used, edges should be securely affixed to the floor with tacks or carpet tape.
A similar problem often arises with door thresholds, the horizontal plank or other surface that forms the bottom edge of a door opening. In particular, exterior thresholds can protrude up to an inch above the interior surface. In such a case, recommend a threshold ramp, available in a variety of materials and rises; it can make crossing door thresholds easier and safer.27 If the home is under construction, the builder may be able to lower the exterior door threshold relative to the interior floor surface (the Center for Universal Design recommends no more than a 1/ 2-in. difference).8 Interior door thresholds should be set flush with surrounding floors.
Bathrooms. Although some people use ordinary bathroom towel bars for balance and support, such bars aren’t designed to support a person’s weight and can collapse or pull out of the wall. The installation of grab bars near bathtubs, showers, and toilets is a frequently recommended modification. (They can also serve as towel holders.) Grab bars should be mounted only to solid lumber behind the drywall. If wall-mounted grab bars can’t be installed near the toilet, adjustable-height grab bars that mount to the toilet base (between the tank and the seat) should be considered.29
Impaired mobility or agility increases the risk of falls in the shower or tub. When needed, a shower chair can be placed in the shower stall or tub, or the existing unit can be replaced by a shower stall with a built-in seat. Installing a movable, hand-held showerhead on a flexible hose and a vertical slide rail with a movable mounting bracket permits people of varying heights to shower easily in seated or standing positions. A shower curtain presents less of a barrier than a shower door. For people who use wheelchairs, construction of a roll-in shower, which has no threshold, is optimal. An elevated toilet seat, low in cost and easy to install, eases transfers by offering seating near the height of most wheelchair seats.8
Stairs. Handrails on both sides of a stairway can be useful; as with grab bars, handrails should be anchored securely to solid lumber behind drywall. A horizontal extension of one or both handrails by several inches at the head and foot of the stairs can provide added support. New stairs can be built with lower-than-standard risers and longer-than-standard treads to improve their navigability and reduce the risk of falls.29 Handrails can also be installed in hallways.
Other areas. Rearrangement of furniture, or replacement or removal of some pieces, can make a home safer and navigation easier. For example, a strategically placed large upholstered chair can be used for support. Conversely, a decorative pedestal table used for support might cause a fall, as might chairs on casters, which can roll unexpectedly. Chairs with arms provide extra support when a person is sitting down or standing up. Lift chairs, featuring a seat-lifting mechanism that raises a person from a seated to a standing position, can be found at home medical supply retailers and furniture manufacturers.
Suggest the use of remote-control devices for lamps, televisions, and other appliances. People who use wheelchairs often find that washers and dryers with front-mounted (rather than top-mounted) controls, and side-by-side refrigerator–freezer units are easier to use than other models. Contrary to what many people believe, appliances that incorporate universal design features are often available from local retailers and don’t necessarily cost more than standard models. Creating open, clear space under countertops and sinks improves access for people who use wheelchairs or prefer to work while seated. Adjustable height kitchen countertops are also an option.
Objects stored in cabinets and closets can be made more accessible with lazy Susans, pull-out and adjustable-height shelves, step stools, and adjustable rods mounted at two levels.
Impaired strength and range of motion. While the patient performs ADLs and IADLs, watch for difficulty bending, reaching, maintaining a standing position, transferring, carrying or moving objects, and opening and closing doors and drawers.
Many modifications suitable for people with impaired mobility or agility, such as installation of grab bars and use of remote-control devices, also benefit those with impaired strength or range of motion. Lever handles require less strength and coordination to use than standard doorknobs and faucets. For the same reason, cabinet doors and drawers should be equipped with loop handles.27, 29
People with impaired strength often prefer to prepare meals while seated, so installing adjustable height kitchen countertops and creating open, clear space under a countertop or sink are appropriate modifications.
If a person has difficulty reaching light switches, the switches can be mounted on walls at a height of 44 to 48 in.8, 27 And because the concealed hinges on typical cabinet doors open only to an angle of slightly more than 90°, they should be replaced with those that open to an angle of at least 180°.29
Impaired sense of touch or dexterity. Scalding from hot tap water is a danger for elderly adults, very young children, and people with impaired dexterity or sense of touch30, 31; impaired agility may also pose a risk. The American Academy of Family Physicians recommends that water heaters be set to a maximum temperature of 120°F; higher temperatures can cause burns in two or three seconds.32 Pressure-balancing valves can compensate for sudden changes in water pressure, and thermostatic mixing valves can regulate temperature; both are recommended in showers, tubs, and sinks to reduce the risk of scalding.8, 27 Combination thermostatic mixing and pressure balancing valves are also available.
Tasks that involve pinching, twisting, or gripping can pose a challenge to people with impaired touch or dexterity; again, lever handles and loop handles can help.27 Johnson and colleagues recommend heightening “the tactile sensation by making the surfaces of walls and counters more distinctive” by using materials such as brick and patterned vinyl.27
Johnson and colleagues have noted that smooth top electric ranges present a particular hazard to this population because elements that are still dangerously hot may no longer glow brightly; they recommend the use of electric ranges with warning lights indicating when a burner is too hot to touch.27 They also recommend that patients consider the accessibility and ease of use of controls when purchasing appliances.27
Impaired hearing. People with noise-induced hearing loss—the most common cause of sensorineural hearing impairment in adults33—have difficulty hearing higher-frequency sounds and certain consonants in speech, as well as understanding speech when background noise is present. The use of telephones, televisions, and radios may be problematic.34, 35
Telephones equipped with speaker and ringer amplification are available. Some models also feature the option of selectively amplifying higher frequency tones.29
For hearing-aid users, selecting telephones and hearing aids that are compatible is recommended. Telephone-compatible hearing aids contain a telecoil, a device that reduces electromagnetic feedback and background noise and limits amplification to the sounds emitted from the handset. Hearing-aid compatible telephones must “produce a magnetic field of sufficient strength and quality to permit coupling with hearing aids that contain telecoils.”36 The Federal Communications Commission has been charged with ensuring that all telephones sold in the United States be hearing-aid compatible and has established timetables by which manufacturers must comply. However, to date many telephones, especially cordless and wireless models, are not compatible.36, 37 Encourage patients who are using older phones and hearing aids to consider upgrading to compatible models.
Television design, particularly speaker placement, affects the way sound is directed. A front mounted speaker, which projects sounds directly to the viewer, is optimal. When the speaker is on the side of the unit, sounds are projected away from the viewer, making it more difficult to hear. The viewer may seek to compensate by increasing the volume, but this often distorts sound. Remote speakers or headphones, either corded or cordless, can be used with televisions equipped with an audio output jack.
Reducing background noise, often from appliances such as air conditioners, refrigerators, and dishwashers, can greatly enhance communication.38 There are models designed for quiet operation; keeping appliances in good repair, installing insulation around them, or moving them may also help.
REMODELING AND NEW HOME CONSTRUCTION
Homeowners planning major remodeling should choose a general contractor who can incorporate universal design features into a given project (for example, remodeling a bathroom). Encourage the patient to prepare a list of specific design features desired (such as grab bars and a roll-in shower), and suggest that the prospective contractor review the list and sign an agreement stating that he will incorporate these features. Similarly, people building new homes should discuss universal design features with prospective builders before choosing one.
Almost any home that has a bedroom and a three-quarter bathroom (toilet, sink, and shower) on the main floor can be made fully accessible for at least one family member. If the home doesn’t already include these features, it may be possible to convert a dining room or other area on the ground floor to a bedroom, and a half bathroom into a three-quarter or full bathroom. Alternatively, a stair lift or elevator may be installed.27
Some families choose to add an “in-law” suite or an accessory apartment to their home. An in-law suite typically consists of a bedroom, bathroom, and sitting room; an accessory apartment has a small kitchen as well. Such arrangements allow older adults with disabilities to stay close to other family members (often less expensive than separate housing) while preserving their independence.
Features that can be readily incorporated into new home construction include wider-than-standard doorways and recessed thresholds. Some groups, such as the Consortium of Multiple Sclerosis Centers, advocate making 36-in. interior doorways standard in all new home construction.39 Encourage patients who are building homes to include such features; they help make a home accessible to anyone with a disability.
Cases revisited. Visiting the local health department for foreign travel immunization, Ms. Thomas mentioned her concerns to a public health nurse about sharing her home with her aging mother. The nurse gave Ms. Thomas some literature on home modification. They discussed several options, including converting a ground-floor office into a bedroom and installing grab bars and a roll-in shower in the ground-floor bathroom. They also discussed managing costs. Ms. Thomas realized she could make simple changes herself, such as replacing doorknobs with lever handles. Other changes would require hiring a local contractor. Although the modifications were related to her mother’s health needs, health insurance covered none of the equipment, materials, or labor costs. She obtained a low-cost home improvement loan. On completion of the project, Ms. Thomas was pleased that the new modifications were unobtrusive; they didn’t diminish the attractiveness of her home and indeed would make it more appealing to future buyers. She felt that the benefits of having her mother nearby, including the savings realized by not having to move her mother to a long-term care facility, were worth the investment.
The Hartfords talked over their plans to build a new house with their son’s home care nurse, who had introduced them to home modification concepts years earlier. She suggested they find a builder who could customize a standard new home design. The Hartfords were interested in a variety of household products advertising their compliance with standards established by the Americans with Disabilities Act of 1990. (For these design standards, see www.usdoj.gov/crt/ada/stdspdf.htm.) The nurse explained that while such products are generally well designed and suitable for use by people with disabilities, many products made for the general public also incorporate universal design features and are often less expensive and available through local retailers.
REFERENCES
1. U.S. Census Bureau. 12th anniversary of Americans With Disabilities Act (July 26). Washington, DC: The Bureau; 2002 Jul 12. CB02-FF.11. http://www.census.gov/Press-Release/ www/2002/cb02ff11.html.
2. Pynoos J, Sanford J. New tools for better home modifications. Case Manager 2002;13(1):67-70.
3. Zola IK. Self, identity and the naming question: reflections on the language of disability. Soc Sci Med 1993;36(2):167-73.
4. Peel N, et al. Home safety assessment in the prevention of falls among older people. Aust N Z J Public Health 2000; 24(5):536-9.
5. Cumming RG, et al. Adherence to occupational therapist recommendations for home modifications for falls prevention. Am J Occup Ther 2001;55(6):641-8.
6. Freedman VA, et al. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA 2002;288(24):3137-46.
7. Mathew Greenwald and Associates. These four walls: Americans 45+ talk about home and community. Washington, DC: AARP; 2003 May. http://assets.aarp.org/rgcenter/il/ four_walls.pdf.
8. Center for Universal Design. Universal design in housing. Raleigh, NC: North Carolina State University; 2006 Feb. http://www.design.ncsu.edu/cud/pubs_p/docs/UDinHousing.pdf.
9. Americans with Disabilities Act of 1990. Public Law No. 101-336. US Statut Large 1990;104:327-78.
10. Richards C. Toward universal access in the workforce development system. Washington, DC: National Collaborative on Workforce and Disability for Youth; 2005 Aug. http://www. ncwd-youth.info/assets/background/Toward_Universal_ Action.pdf.
11. Housing Research Foundation. Visitability improves accessibility for all. Hope VI Developments Newsletter 2000 (41). http://www.housingresearch.org/hrf/HRF_News.nsf/ea83fb17 e8038680852569d0000d00b6/b0003c82ff472199852569d0 0010e8bc!OpenDocument&Highlight=2,visitability&Click=.
12. Smith E. Visitability defined. 2003 Nov. http://www. concretechange.org/Definition_of_Visitability.htm.
13. Tinetti ME, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 1994;331(13):821-7.
14. Close J, et al. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet 1999;353(9147):93-7.
15. Cumming RG, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc 1999;47(12):1397-402.
16. Nikolaus T, Bach M. Preventing falls in community-dwelling frail older people using a home intervention team (HIT): results from the randomized Falls-HIT trial. J Am Geriatr Soc 2003;51(3):300-5.
17. Gitlin LN, et al. A randomized, controlled trial of a home environmental intervention: effect on efficacy and upset in caregivers and on daily function of persons with dementia. Gerontologist 2001;41(1):4-14.
18. Kutty NK. The production of functionality by the elderly: a household production function approach. Appl Econ 2000; 32(10):1269-80.
19. Gitlin LN, et al. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc 2006;54(5):809-16.
20. Salkeld G, et al. The cost effectiveness of a home hazard reduction program to reduce falls among older persons. Aust N Z J Public Health 2000;24(3):265-71.
21. Ogden CL, et al. Mean body weight, height, and body mass index, United States 1960-2002. Adv Data 2004(347):1-17.
22. Gibson MJ, et al. Beyond 50.03: a report to the nation on independent living and disability. Washington, DC: AARP Public Policy Institute; 2003 Apr. Pub ID: D17817. http:// www.aarp.org/research/housing-mobility/homecare/ aresearch-import-752-D17817.html.
23. Kochera A. In brief: falls among older persons and the role of the home: an analysis of cost, incidence, and potential savings from home modification. Washington. DC: AARP; 2002 Mar. INB No. 49. http://assets.aarp.org/rgcenter/il/ inb49_falls.pdf.
24. Reid D, et al. Home is where their wheels are: experiences of women wheelchair users. Am J Occup Ther 2003;57(2): 186-95.
25. Josephson KR, et al. Home safety and fall prevention. Clin Geriatr Med 1991;7(4):707-31.
26. Extended Home Living Services Inc. Comprehensive assessment and solution process for aging residents. Wheeling, IL: The Services. http://www.ecaspar.com/ec/caspar.pdf.
27. Johnson M, et al. Home modifications and products for safety and ease of use. Raleigh, NC: Center for Universal Design, North Carolina State University; 1999. http://www. design.ncsu.edu/cud/pubs_p/docs/Home%20Modifications% 20and%20Products.pdf.
28. AARP. Doors, floors, and walkways. http://www.aarp.org/ families/home_design/doors_floors/a2004-03-02-d-hallways. html.
29. Bakker R. Elderdesign: designing and furnishing a home for your later years. New York: Penguin Books; 1997.
30. Stone M, et al. The continuing risk of domestic hot water scalds to the elderly. Burns 2000;26(4):347-50.
31. Wibbenmeyer LA, et al. Population-based assessment of burn injury in southern Iowa: identification of children and young-adult at-risk groups and behaviors. J Burn Care Rehabil 2003;24(4):192-202.
32. American Academy of Family Physicians. Burns: preventing burns in your home. 2005 Sep. http://familydoctor.org/649. xml.
33. Holt J, et al. Demographic aspects of hearing impairment: questions and answers 3rd ed. Washington, DC: Gallaudet University; 1994. http://gri.gallaudet.edu/Demographics/ factsheet.html.
34. Hetu R, et al. The impact of acquired hearing impairment on intimate relationships: implications for rehabilitation. Audiology 1993;32(6):363-81. 35. Hetu R, et al. Impact of occupational hearing loss on the lives of workers. Occup Med 1995;10(3):495-512.
36. Federal Communications Commission. Hearing aid compatibility for telephone equipment. 2006. http://www.fcc.gov/ cgb/consumerfacts/hac.html.
37. Mayo Clinic. Hearing aids: how to choose the right one. 2005 Mar 31. http://www.mayoclinic.com/health/hearing-aids/ HQ00812.
38. National Institute on Deafness and Other Communication Disorders. Presbycusis; 1997 Oct. NIH Pub. No. 97-4235. http://www.nidcd.nih.gov/health/hearing/presbycusis.htm.
39. Gackle C. Home accessibility = greater independence. Teaneck, NJ: Consortium of Multiple Sclerosis Centers; 2003 Aug. http://www.mscare.org/cmsc/images/pdf/ HomeAccessibility-Gackle.pdf.
