Headache in Multiple Sclerosis
Why is this important to me?
People with MS have a high incidence of headaches, but the details of the relationship between the two conditions is unclear. Headaches may be different depending on the subtype of MS and the location of lesions in the brain. Several MS medications can worsen headaches, causing patients to not take their medications. Headache management in people with MS will improve quality of life.
What is the objective of this study?
MS patients who experienced headaches were questioned about their headache history, pain, headache triggers, relationship with MS disease progression, and effect of headaches on their quality of life and daily functioning. Results of the survey showed:
- Two-thirds of MS patients experienced headaches before MS symptoms began.
- Duration and severity: Half the patients had headaches at least once a week, with most being severe. Around half the patients had headaches that lasted more than 4 hours if they did not take medication for headache pain. Headaches tended to worsen if MS was also worsening.
- Migraine: Almost half of patients reported migraine with aura, and these headaches tended to worsen during times when their MS was worsening. Auras most frequently included dizziness and blurred vision.
- Description of pain: About half of MS patients with headaches reported that the pain was sharp, stabbing, or throbbing. Patients who report that their headaches worsen when MS is worsening, when they are stressed, or during an episode of fatigue describe sharp pain.
- Headache triggers: The most common headache triggers reported in this group of MS patients were stress and fatigue, followed by bright lights, loud noises, menstrual periods, and high-salt foods. Of these, only fatigue was associated with headaches worsening when MS symptoms were worsening. Headaches were not worse during pregnancy. Alcohol, tobacco, and caffeine consumption did not affect headache characteristics.
- Daily functioning: Headaches sometimes required patients to rest, reducing their ability to perform daily activities.
Headaches may impact your quality of life, including your daily activities, mood, and ability to concentrate. Two main triggers of headaches, stress and fatigue, can be improved with behavioral changes, and addressing these triggers may alleviate your headaches. Learning how to identify and avoid other triggers may also help prevent headaches and improve quality of life. If you experience migraines with auras or sharp pain, these may be early indicators of MS worsening, and you should be evaluated for this possibility so that you can be treated sooner. You should be assessed for headaches during clinical visits for your MS, and a customized plan aimed at minimizing headaches may be helpful.
How did the authors study this issue?
The authors enrolled 72 patients with MS who also reported headaches. Participants answered questionnaires designed to assess various characteristics of headaches and the relationship between headaches and MS features. Most participants were women.
Original Article
Headache in Multiple Sclerosis Features and Implications for Disease Management
International Journal of MS Care
David Tabby, DO; Muhammad Hassan Majeed, MD; Branden Youngman, DO; Jessica Wilcox, BS
People with multiple sclerosis (MS) have an increased incidence of headaches, although the comorbidity of headaches and MS is poorly understood.1 Lifetime prevalence appears to be highly variable, with reports ranging from 4% to 58%.2–7Despite the inconsistency of prevalence reporting, there is clinical value in the identification of headache incidence in MS patients.2,8,9 Evidence suggests that headaches may vary based on MS form and lesion location, and MS patients with migraines have a more symptomatic clinical course of the disease.8 In addition, screening patients with MS for headaches has treatment implications. Several medications used to treat MS have been shown to exacerbate headaches, leading to a decreased quality of life and possible treatment nonadherence.8
Owing to the highly variable presentation of headaches in patients with MS, much remains to be elucidated about the variables affecting headache development. We analyzed a number of factors in relation to headache incidence in a sample of our patients with MS, focusing on headache history, pain description, modifying factors, social history, relation to disease progression, and impact on quality of life.
Materials and Methods
Questionnaire Distribution
In a prospective study at the Drexel University College of Medicine Multiple Sclerosis Program, 72 patients with both MS and headaches anonymously completed a 28-item questionnaire (Appendix 1). Only MS patients with a self-identified history of headaches were asked to participate. For one 6-month period, patients were invited to complete this survey in the waiting room and through e-mail. To ensure anonymity, no names or other patient identifiers were recorded. From the responses, we examined in detail each patient's demographics, drug and alcohol use, headache characteristics, frequency, location, duration, pain description, modifying factors, triggers, and impact on patient functioning. We also assessed headache features in relation to MS diagnosis, disease exacerbations, and physiological conditions such as pregnancy and menses.
Statistical Analysis
One-sample binomial and χ2 tests were used to describe the significance of each variable independently. Bivariate comparisons of all groups were then performed using Pearson correlations and the Fisher exact test. Findings with two-tailed P values less than .05 were considered significant. Analysis was performed with SPSS Statistics for Macintosh, version 19 (IBM, Armonk, NY).
This study received approval from the Drexel University College of Medicine Institutional Review Board.
Results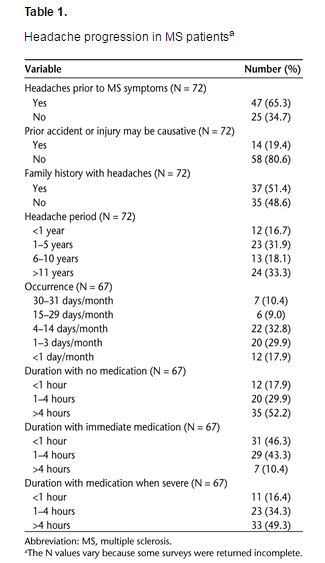
Headache Progression
Two-thirds of patients reported the presence of headaches before the start of their MS symptoms (P < .013) (Table 1). Although only 19% suffered an injury that may have caused headache initiation, half of the patients reported a family history of headaches, unrelated to familial MS incidence. Half of the patients in our sample reported that they had headaches at least once a week (P < .001), with the majority stating that their headaches were severe at least some of the time. In connection with this severity, 52% of the patients reported that their headaches lasted for more than 4 hours without medication (P < .001). If they took medication immediately after headache onset, many patients reported a reduction in headache duration (P < .001), although for 10% headaches continued to last for more than 4 hours. Among patients who waited until headaches became severe to take medication, far fewer received considerable benefits in headache reduction.
Migraine with Aura
Forty-three percent of our patients experienced migraine with aura (Table 2). Of these auras, the most common symptoms were dizziness, blurred vision, and tightness. (Tightness as an aura refers to a tight sensation in the posterior cervical and cranial muscles indicating an impending migraine.) Roughly one-third of patients reported other visual disturbances, including halos around lights, flashing lights, and blind spots. There was a statistically significant inverse relationship between aura occurrence and headache incidence before MS (P < .015). Of the patients with no headache history prior to MS onset, 64% experienced migraine with aura as the disease progressed. Conversely, auras were present in only 34% of the patients who did have a preceding history of headaches. Furthermore, patients who reported auras were more likely to state that their headaches were worse during MS exacerbations (P < .003). Visual disturbances, such as blurred vision and halos, were highly correlated with longer duration of headaches (P < .005) and with limiting activities of daily living (P < .02). None of the other auras had a statistically significant relationship with headache duration.
Pain Description
MS patients in our sample reported pain of 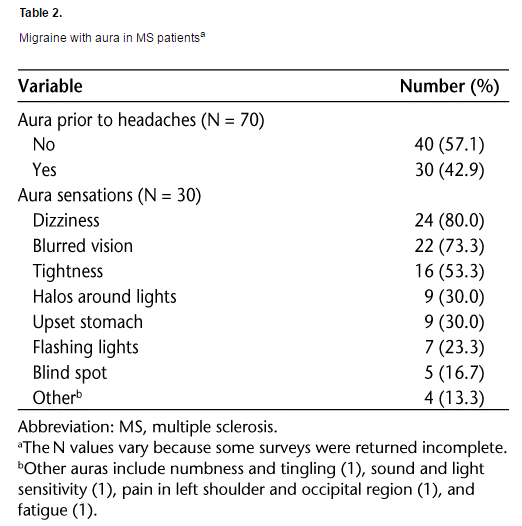 varying types (Table 3). Throbbing, sharp, and stabbing headaches were described by close to 50% of all MS patients in this study. Dull pain was reported by 28% of patients, and a tight band or burning feeling occurred in fewer than 20% of patients. Variation was reported not only among patients but also between headache attacks in the same patient. Roughly equal percentages of patients (18–24%) reported headaches occurring in the left, right, or either hemisphere. A slightly elevated number (36%) had headaches on both sides. Throbbing pain was more commonly associated with long headache history (P < .05) and with more frequent headache occurrences (P < .002). Patients who reported sharp pain were more likely to report headache worsening during MS exacerbations (P < .04). Sharp pain was also significantly associated with stress and fatigue triggers (P < .001 and P < .01, respectively).
varying types (Table 3). Throbbing, sharp, and stabbing headaches were described by close to 50% of all MS patients in this study. Dull pain was reported by 28% of patients, and a tight band or burning feeling occurred in fewer than 20% of patients. Variation was reported not only among patients but also between headache attacks in the same patient. Roughly equal percentages of patients (18–24%) reported headaches occurring in the left, right, or either hemisphere. A slightly elevated number (36%) had headaches on both sides. Throbbing pain was more commonly associated with long headache history (P < .05) and with more frequent headache occurrences (P < .002). Patients who reported sharp pain were more likely to report headache worsening during MS exacerbations (P < .04). Sharp pain was also significantly associated with stress and fatigue triggers (P < .001 and P < .01, respectively).
Modifying Factors
We selected triggers that many of our patients reported historically as options for this survey and left space for the patients to note any additional triggers. The most common triggers of headache were stress (78%, P < .001) and fatigue (64%, P < .02), although bright lights, loud noises, menstruation, and certain foods (namely, those high in sodium) also affected a large number of people (Table 4). Headaches stemming from stress and fatigue were most likely to present as sharp or stabbing pain (noted above) and require rest (P < .02). Fatigue was the only trigger associated with headache worsening during MS exacerbations (P < .003). MS exacerbations caused a worsening of headaches for nearly two-thirds of our patients (P < .05). Most patients reported no change in headache severity between seasons, although one-fifth reported more severe headaches during the summer.
Approximately half of the premenopausal women described a worsening of headaches during menstruation. No women reported any increase in headache severity during pregnancy, and 12% reported 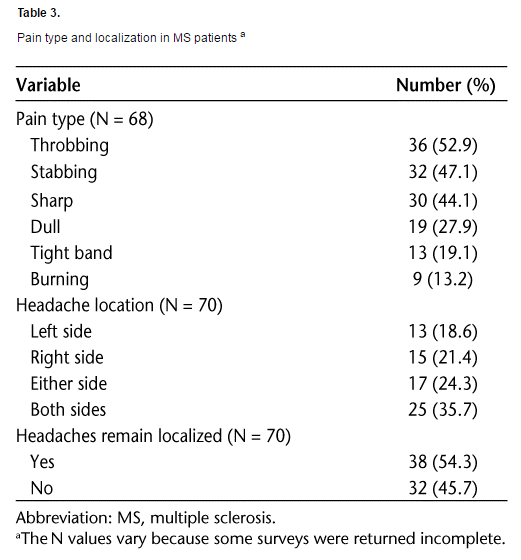 a reduction of headache symptoms while pregnant.
a reduction of headache symptoms while pregnant.
Impact on Daily Function
The influence of headaches on daily functioning reported by our patients followed a normal distribution (Table 5). Fatigue, irritability, difficulty concentrating, and limitation of daily activities were reported by 24% to 34% of MS patients some of the time, with generally fewer reporting more or less frequent occurrences. The most significant finding correlates with the increased severity of headaches reported by MS patients, with 39% of the patients requiring rest every time they experienced a headache (P < .001). An additional 21% reported needing to lie down very frequently. The vast majority of patients, 85%, experienced severe headaches at least some of the time, and 43% reported that their headaches were severe very often or always (P < .001).
Headaches and Social History
We found no statistically significant correlations between headache characteristics when we controlled for alcohol, tobacco, and caffeine usage (Table 6).
Discussion
Headache presentation was variable among our sample of MS patients. Sixty-five percent of our patients reported that their headaches began prior to MS onset. This relationship raises two questions: 1) Could 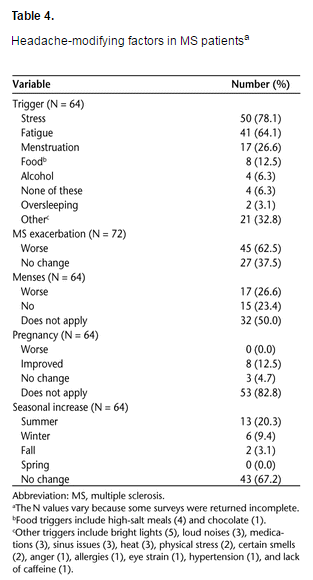 headache be a presenting symptom of MS? and 2) Is headache a treatable risk factor for MS? Other studies have found similar presentations of headaches, most notably migraines, prior to MS onset. The Nurses’ Health Study II found a 47% increase in relative risk for MS development in nurses with migraines as opposed to those without migraines, although the difference in absolute risk was small.9 One proposed mechanism is that migraines, specifically those with auras, can induce activation of matrix metalloproteinases, resulting in increased permeability of the blood-brain barrier.10 This allows for exposure of central nervous system antigens to circulating T cells, potentially facilitating the autoimmune demyelination that is the hallmark of MS.
headache be a presenting symptom of MS? and 2) Is headache a treatable risk factor for MS? Other studies have found similar presentations of headaches, most notably migraines, prior to MS onset. The Nurses’ Health Study II found a 47% increase in relative risk for MS development in nurses with migraines as opposed to those without migraines, although the difference in absolute risk was small.9 One proposed mechanism is that migraines, specifically those with auras, can induce activation of matrix metalloproteinases, resulting in increased permeability of the blood-brain barrier.10 This allows for exposure of central nervous system antigens to circulating T cells, potentially facilitating the autoimmune demyelination that is the hallmark of MS.
Only one-third of our patients who had headaches before MS onset had migraine with aura. However, twothirds of the patients who did not experience headaches before MS reported the presence of auras. Because headache causation for these patients is likely to be associated with their disease, this strong association with auras may shed light on the hypothesized causal pathway between migraines with auras and MS. Furthermore, our patients with auras were more likely to report headache worsening during self-reported MS exacerbations. This association raises the possibility that auras could be an early marker for MS exacerbations, which if confirmed might allow for earlier treatment and better management.
There are several hypotheses regarding how headache results from various forms of MS pathogenesis. These mechanisms include decreased serotonin in the cerebrospinal fluid, sympathetic hypofunction, and cytokine changes.11 The relationship of headache subtypes with MS course and lesion sites has been studied. Migraines have been associated with lesions in the brainstem, C2 dorsal horn, and periaqueductal gray matter.12 In addition, several studies have shown migraines to be more common in patients with relapsing-remitting MS, and tension-type headaches to occur more frequently in the secondary progressive form.2 However, the implications of tension-type headaches in MS are questionable. Current epidemiological studies have not provided convincing evidence that tension-type headaches are more frequent in MS patients compared with the general population, although large-scale investigations of this headache subtype are lacking.13 Another study has correlated primary stabbing headaches with the relapse phase of relapsing-remitting MS, implicating stabbing pain as a potential sign of acute demyelination.14
The pain described by the patients in our study varied based on headache frequency, history, and MS progression. Patients who had a long or frequent history of headaches were more likely to report their pain as throbbing. Sharp and stabbing headaches were highly associated with headache worsening during MS exacerbations. These observations strengthen the previous findings that primary stabbing headaches may signify an acute demyelination episode.
Another hypothesis suggests that MS and headache, particularly migraines, develop as a result of a shared factor, such as a common environmental and/or genetic link that fluctuates with endocrine changes. One observation that supports this hypothesis is that both MS activity and migraine frequency were reduced in pregnancy.8 Our findings are consistent with the common observation that headaches worsen during menstruation and tend to decline during pregnancy. Twenty-seven percent of our sample indicated headache exacerbations during menses. Of the 11 women who indicated a history of pregnancy in the survey, 8 reported a reduction in headache incidence during pregnancy, and the other 3 indicated no change in headache severity. No women reported a worsening of headaches during pregnancy.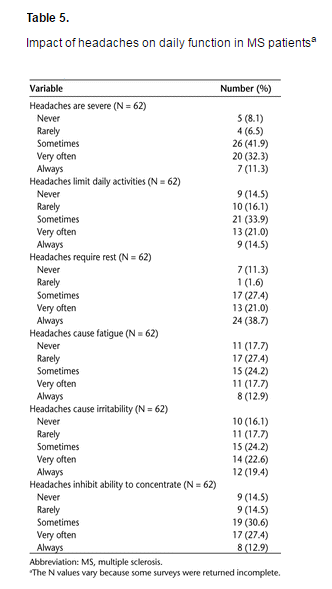
In order to limit patient identifiers, we did not directly address gender in this survey, but the clinic demographic is 88% women. While MS and migraine are both known to affect more women than men, very few data exist on other differences in headache presentation between men and women with MS. Given the predominance of women among those who develop migraines, it is possible that men who experience such headaches are at a higher risk for a severe course of disease. A few studies have shown tension-type headaches to be slightly more common in men with MS than in women with MS,1,2 although the reason behind this observation is unclear. Considering the hormonal influences on both headache and MS, further studies are warranted to determine whether gender differences influence the course of headache presentation and disease severity.
Headache severity in our patients correlated with headache worsening during MS exacerbations. Of the patients whose headaches were frequently to always severe, 85% also reported that their headaches were worse during MS exacerbations. Conversely, only 11% of patients who never or rarely experienced severe headaches had worsening upon MS flare-ups. Migraineurs have been shown to have a worse symptomatic clinical course as well, regardless of migraine frequency or severity. This includes reports of an increased history of depression, episodic neurologic dysfunction, pain-related symptoms, and side effects of interferon treatment compared with MS patients without migraine.8
These findings may be attributed to the observation that debilitating headaches, such as migraines, trigger more severe inflammation in the brain, prompting a positive relationship between headache severity and the degree of disability. Another explanation is that increased frequency of severe headaches induces a central sensitization and a lowering of pain threshold for each degree of lesion-induced disability.
The increase of headache severity with MS exacerbations may also explain, in part, why MS patients are more likely to report greater headache severity in the summer than at any other time of the year. Thirteen patients reported increases in headache symptoms in the summer, although only three patients identified heat as a trigger. According to Uhthoff’s phenomenon, neurologic symptoms of demyelination worsen when the body becomes overheated. The proposed mechanism for this finding is that increased temperature inhibits nerve conduction in damaged nerves, even when symptoms may not be apparent at normal body temperatures. This “disability unmasking” has already been shown to influence fatigue, pain, concentration, and urinary urgency in patients with MS.15 With emerging data identifying headache as a common symptom of MS, it would be interesting to study the effect of heat on headache development in these patients.
Headache presence and severity have clinical implications in patients with MS. Not only could these data provide clues regarding MS course and exacerbations, but they may also have implications for patients’ quality of life.8 Our patients reported that headache affected their daily activities, mood, and ability to concentrate. More than half reported pain so intense it required them to rest until the pain subsided, further hampering patient functioning. This observation is strikingly similar t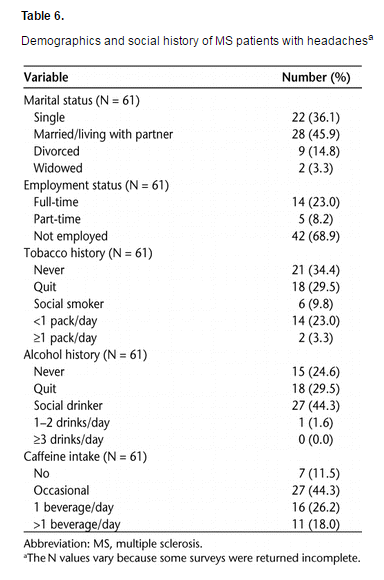 o the estimates of disability in chronic migraine sufferers, of whom more than 50% experience severe impairment during headaches.16 Unfortunately, several treatments exacerbate headaches in patients with MS, particularly those with migraine. Sixty-nine percent of the patients surveyed, all of whom were diagnosed with MS and had comorbid headaches, were not employed. All these factors can impair a patient’s ability to sustain steady employment, resulting in economic burden to the health-care system as well as to social services.
o the estimates of disability in chronic migraine sufferers, of whom more than 50% experience severe impairment during headaches.16 Unfortunately, several treatments exacerbate headaches in patients with MS, particularly those with migraine. Sixty-nine percent of the patients surveyed, all of whom were diagnosed with MS and had comorbid headaches, were not employed. All these factors can impair a patient’s ability to sustain steady employment, resulting in economic burden to the health-care system as well as to social services.
Fortunately, for some the incidence of headache may be reduced using a multidisciplinary treatment approach. The greatest identifiable triggers for headache in this study were stress and fatigue, both of which can be alleviated with counseling and behavioral management. These triggers were closely associated with the sharp and stabbing headaches that are known to heighten during MS exacerbations. As stress and fatigue are also symptoms of MS exacerbations, the causal pathway in this situation is unclear. Is headache worsening caused by stress and fatigue secondary to MS flare-ups, or is headache a side effect of the cytokine changes that occur during demyelinating episodes? Furthermore, psychological stress has long been shown to precipitate MS exacerbations.17 If these triggers can be alleviated, the severity of MS exacerbations may subside as well. Other preventable triggers include chocolate, high-salt foods, heat, and alcohol. If we can help MS patients identify and avoid headache triggers, we can help prevent headaches and improve quality of life.
Study Limitations
Our study has several limitations. Because we did not survey MS patients without headaches, we cannot deduce the incidence of headaches in our total patient population. However, several other studies have shown a highly variable trend.2-7 We did not collect data regarding current medications, such as beta-interferon therapy or specific headache management drugs, which may influence the course of headache presentation. In order to reduce questionnaire length and encourage participation, headache subtype and stage of MS were not included in the survey. Self-identification of these two variables might have led to misinterpretation of results, and appropriate classification of these components would have required access to patient medical records, which were excluded to preserve anonymity. For the same reason, we cannot confirm the authenticity of patient reported MS exacerbations or analyze the data according to radiologic findings. However, brain imaging was not necessary for the purposes of this study, which focused on determining the history and characteristics of headaches in MS patients rather than the relationship to specific lesion sites. Finally, the patients chosen for this study were selected from the Drexel University College of Medicine Multiple Sclerosis Program, a population that skews slightly toward the severe end of the disability spectrum.
Conclusion
Comorbid headaches in MS are too detrimental to patient functioning and quality of life to be ignored. Despite the variability in reported prevalence, the connection between MS progression and headache patterns is evident and calls for the inclusion of headache inquiry in the examination of all patients with MS. Investigating the determinants of headache development and severity can allow for improved management of MS through several possible means, including 1) decreased headache frequency; 2) improved quality of life; 3) reduction in health-care costs; 4) for some patients, an increased ability to remain employed; 5) increased treatment effectiveness and compliance; and 6) for some patients, a change in the symptomatic course of MS.
In these patients, a tailored therapeutic approach may be indicated. MS patients experiencing migraines with aura and sharp pain should be evaluated for MS relapse, so the appropriate treatment may be implemented. Preventable headache triggers, most commonly stress and fatigue, should be evaluated to reduce headache attacks and improve patient functioning. Neurologists should consider a multidisciplinary approach to MS treatment that includes a thorough analysis of headache history in order to best control MS symptoms, determine the most appropriate treatment, and improve patient quality of life.
Further research in this area is warranted to investigate the physiological correlation between MS and headaches. The time course of headache development as it relates to MS exacerbations should be evaluated to determine whether headache precedes demyelination symptoms or vice versa. A stronger understanding of this causal pathway may elucidate the implications of auras and pain description during MS progression. Long-term studies should be conducted to determine whether treating headaches promptly and aggressively affects the clinical course of MS and the level of patient functioning.
References
1. Villani V, Prosperini L, Pozzilli C, et al. The use of ID migraineTM questionnaire in patients with multiple sclerosis. Neurol Sci. 2011;32: 269–273.
2. D’Amico D, La Mantia L, Rigamonti A, et al. Prevalence of primary headaches in people with multiple sclerosis. Cephalalgia. 2004;24:980–984.
3. Watkins SM, Espir M. Migraine and multiple sclerosis. J Neurol Neurosurg Psychiatry. 1969;32:35–37.
4. Clifford DB, Trotter JL. Pain in multiple sclerosis. Arch Neurol. 1984;41:1270–1272.
5. Freedman MS, Gray TA. Vascular headache: a presenting symptom of multiple sclerosis. Can J Neurol Sci. 1989;16:63–66.
6. Rolak LA, Brown S. Headaches and multiple sclerosis: a clinical study and review of the literature. J Neurol. 1990;237:300–302.
7. Pollmann W, Erasmus LP, Feneberg W, et al. Interferon beta but not glatiramer acetate therapy aggravates headaches in MS. Neurology. 2002;59:636–639.
8. Kister I, Caminero AB, Monteith TS, et al. Migraine is comorbid with multiple sclerosis and associated with a more symptomatic MS course. J Headache Pain. 2010;11:417–425.
9. Kister I, Munger KL, Herbert J, Ascherio A. Increased risk of multiple sclerosis among women with migraine in the Nurses’ Health Study II. Mult Scler. 2012;18:90–97.
10. Gursoy-Ozdemir Y, Qiu J, Matsuoka N, et al. Cortical spreading depression activates and upregulates MMP-9. J Clin Invest. 2004;113:1447–1455.
11. Elliott DG. Migraine in multiple sclerosis. Int Rev Neurobiol. 2007;79:281–302.
12. Putzki N, Katsarava Z. Headache in multiple sclerosis. Curr Pain Headache Rep. 2010;14:316–320.
13. Kister I, Caminero AB, Herbert J, Lipton RB. Tension-type headache and migraine in multiple sclerosis. Curr Pain Headache Rep. 2010;14:441–448.
14. Ergün U, Ozer G, Sekercan S, et al. Headaches in the different phases of relapsing-remitting multiple sclerosis: a tendency for stabbing headaches during relapses. Neurologist. 2009;15:212–216.
15. Flensner G, Ek AC, Söderhamn O, Landtblom AM. Sensitivity to heat in MS patients: a factor strongly influencing symptomology—an explorative survey. BMC Neurol. 2011;11:27.
16. Lipton RB, Bigal ME, Diamond M, et al.; AMPP Advisory Group. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343–349.
17. Mohr DC, Hart SL, Julian L, Cox D, Pelletier D. Association between stressful life events and exacerbation in multiple sclerosis: a metaanalysis. BMJ. 2004;328:731–736.
