Self-Management of Urinary and Fecal Incontinence
Why is this important to me?
Many people with MS experience bladder and/or bowel incontinence, which can be physically, emotionally, and psychologically stressful. Skin irritation, embarrassment, and social isolation are some consequences of incontinence. One strategy for addressing incontinence is called self-management. Nurses and other health professionals can assist patients with learning to self-manage incontinence, thus empowering the patient.
Who will benefit from reading this study/article?
Although this article is not specifically about patients with MS, it reviews strategies for self-management of incontinence that can be utilized by those with MS.
What is the objective of this study?
Self-management depends on “self-efficacy” of the patient, which means that the patient becomes confident in his or her ability to perform certain activities that produce a desired result. Self-efficacy develops over time. Self-efficacy can be encouraged when nurses:
- Mention the relationship between a behavior change and success
- Encourage effort and persistence
- Help to identify any new problems
- Encourage patients to attend support groups with patients with similar problems. Person-to-person interactions are generally more successful than simply providing general information.
- Help struggling patients find a solution
Self-management of incontinence requires understanding the cause of it. Patients with a chronic condition become experts in managing their condition. A patient who successfully self-manages a chronic condition:
- Learns about the condition and takes responsibility for what is needed
- Makes use of resources that provide support
- Accepts the “new normal” of the condition
Six specific behaviors should be adapted if you wish to self-manage any incontinence problems you may be experiencing:
- Identify the problem. You should identify and acknowledge the problem. Then you can set a realistic goal such as going out with friends when desired or traveling.
- Seek evidence-based information (results derived from rigorous scientific research). You should learn about the various valid options for managing incontinence, discuss them with a nurse, and make informed decisions. Patients who make evidence-based decisions are more likely to attain control of their symptoms and less likely to make a harmful choice such as severely limiting liquid consumption.
- Make decisions about using resources and interventions. A nurse can describe available resources to you, explain medical information, and describe what is involved with the various treatments available. Open communication between a nurse and patient can help reduce the embarrassment of admitting an incontinence problem.
- Develop and implement a plan of action. After choosing one or more therapies or behavior changes, a detailed, realistic plan of action with a definitive timeline is needed. For example, pelvic floor muscle exercises of a particular duration may have been chosen. Action plans should be flexible if revisions are needed due to unexpected circumstances.
- Self-monitor the results. A timeline for assessing the results of the action plan are needed. You should learn to recognize changes in your body as a result of the action plan. For example, you may wish to record the type and volume of drinks consumed and the number of times you urinate or have an accident in a certain period of time. If you experience fecal incontinence, you may need to identify problem foods that increase fecal incontinence.
- Set and assess goals. You should set realistic goals and honestly assess the outcome. If the plan was successful, you can continue with it. If goals were not met, readjustment of goals or the plan of action may be needed. Nurses can help manage this assessment and provide support. Over time, symptoms may return or worsen, even with a previously successful plan of action, and adjustment of the self-management plan may be needed.
Some strategies for managing urinary incontinence include:
- Modifying fluid intake, including avoidance of caffeine and not drinking too much fluid
- Various pelvic floor muscle exercises to strengthen the muscles around the urethra
- Bladder training to increase the time between urinations
- Weight management. Weight loss of 5-10% often improves incontinence.
- Constipation management, because straining worsens urinary incontinence.
Some strategies for managing fecal incontinence include:
- Dietary modification
- Keeping a change of underwear nearby
- Identifying the location of public restrooms
- Anti-diarrheal medication is especially helpful for controlling fecal incontinence in men and women with MS.
How did the authors study this issue?
The authors describe the elements of self-management of urinary and/or fecal incontinence and how nurses and other healthcare professionals can assist patients in developing a personalized strategy. The article is geared towards all patients with incontinence regardless of the reason for it.
| SHARE: | |||||
Original Article
Self-Management of Urinary and Fecal Incontinence
Employing evidence-based strategies can help patients take better control
American Journal of Nursing
Wilde, Mary H. PhD, RN; Bliss, Donna Z. PhD, RN, FAAN, FGSA; Booth, Joanne PhD, RN; Cheater, Francine M. PhD, RN; Tannenbaum, Cara MD, MSc
Both urinary and fecal incontinence can have distressing physical, emotional, and psychosocial consequences, including loss of skin integrity due to persistent wetness or irritation from feces, embarrassment brought on by soiled clothing or odor, and self-imposed social isolation. Nevertheless, only 15% to 20% of patients with urinary incontinence and 43% of those with fecal incontinence seek professional care for the problem.1-3 Instead, they try to cope with the condition on their own, with variable success.1, 4
An alternative to patient trial and error is patient self-management, in which nurses and other health care professionals help patients identify problems, make decisions, set goals, take appropriate actions, and modify these actions as circumstances change.5, 6 Self-management can increase patients’ awareness of physical symptoms, empower patients to monitor the effects of behavioral changes aimed at improving chronic conditions, and help them feel better equipped to cope with an illness. While self-management is widely accepted as a means of coping with such chronic health conditions as diabetes, asthma, and arthritis, its value in treating urinary and fecal incontinence is not fully appreciated by many health care providers, who may be aware of the daily challenges faced by those with these conditions, but unsure of how to best support patients in effective self-management.
This article discusses the principles of self-management and their application in treating urinary and fecal incontinence. It describes the benefits realized by patients who apply self-management techniques to address incontinence and, through a case scenario, illustrates the nurse's role in imparting self-management skills to patients and reinforcing their use.
THE KEY ELEMENTS OF SELF-MANAGEMENT
Self-management is a critical component of self-care that requires the patient to monitor and manage symptoms as well as “functional, emotional, psychosocial, and physical” aspects of a chronic illness.7 Self-management largely depends on the development of self-efficacy—that is, on patients’ belief in their ability to perform specific self-care activities and produce a desired result.7 Self-management interventions are most successful when patients participate in a collaborative process of care, and both patient and health care provider share responsibility for the outcomes.5, 6
A qualitative metasynthesis of self-management literature identified the following three processes as essential to successful self-management of a chronic illness 8:
- focusing on illness needs by learning about the illness and taking responsibility for meeting related health care needs
- making use of resources for health care, as well as psychological, spiritual, social, and environmental support
- living with the chronic illness by processing emotions, adjusting to the illness and the “new normal,” making practical lifestyle modifications, and striving for personal growth and satisfaction
Echoing a similar theme, one theory of self-care in chronic illness emphasizes that it is crucial for patients to make evidence-based decisions and to thoroughly evaluate a variety of intervention options.9
In providing support for patients’ self-management, it's important to consider the context of care and the power dynamics associated with the traditional, paternalistic, biomedical model of health care.10, 11 In other words, patients with a chronic disease are likely to develop some expertise in managing their illness, and when nurses encourage that, rather than viewing the patient as “noncompliant, questioning, or know it all,” nurses support self-management.11 However, it is important to bear in mind that numerous factors influence patients’ self-management capacity, and patients cannot be expected to manage a chronic condition entirely on their own.
SELF-MANAGING INCONTINENCE
In the self-management of urinary or fecal incontinence, a precondition for success is the proper treatment of any underlying etiologies. Patients’ self-management behaviors then operate as if in a feedback loop, with patients becoming more knowledgeable about their needs and the management strategies that work best for them.12 In the context of incontinence, six specific self-management behaviors come into play:
- identifying the problem
- seeking evidence-based knowledge
- making decisions about resource use and interventions
- developing and implementing an action plan
- self-monitoring
- setting and attaining goals
Self-efficacy supports self-management behaviors, and each behavior, in turn, promotes self-efficacy (see Figure 1).
Figure 1. Self-management begins with a patient-identified problem. The self-management behaviors that address the problem operate as if in a feedback loop, with patients becoming increasingly knowledgeable about their needs and the strategies that work best for them as they come closer to attaining each goal. Self-efficacy supports self-management behaviors, and each behavior, in turn, promotes self-efficacy.
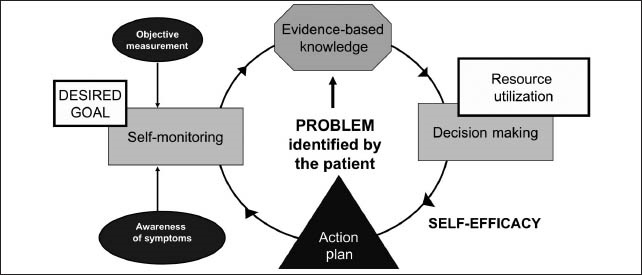
Diagram developed by Cara Tannenbaum.
Identifying the problem. At the center of self-management is a patient-identified problem. Patients need to identify or, as is often the case with incontinence, acknowledge the health problem that needs resolution.
If nurses encourage patients to think about the problem in a way that is meaningful to them and linked to daily activities, it can help them set realistic goals. For example, patients with fecal incontinence might consider whether the scarcity of public restrooms and the fear of soiled clothing or associated odor have caused them to curtail activities outside of the home. This realization may suggest a goal, such as going out with friends when desired.
Seeking evidence-based knowledge. When patients learn about the range of interventions used to manage incontinence, discussing their use and effectiveness with a nurse can help patients make informed choices about how to manage their condition. Patients whose self-management techniques are evidence based are more likely to develop symptom control, which fosters self-efficacy and reinforces the continued practice of such techniques. Without a health care provider's support in learning about evidence-based interventions, patients may initiate harmful strategies such as severely limiting fluid intake, which may put them at risk for dehydration or urinary tract infection.13
Making decisions about resource use and interventions. Although the self-managing patient must ultimately be the one to decide to implement one evidence-based intervention over another, the nurse can inform the patient of appropriate available resources and explain clinical information and differences among treatment alternatives. Concerns about privacy and stigma may keep incontinent patients from asking for guidance from health care providers, but conveying a positive, supportive attitude, and practicing therapeutic communication skills—such as reflective listening, in which the nurse carefully listens to the patient and then paraphrases back what was said to confirm that the nurse understood it—may foster open communication and help patients overcome the embarrassment of acknowledging incontinence. In addition, sharing strategies found useful by others may reassure patients that their problem isn't unique to them.
Guidance is best offered after an in-depth discussion in which the nurse determines the patient's health literacy level, preferences, motivation, and available resources. Nurses should encourage patients to avail themselves of appropriate resources over the course of their chronic condition and to seek continuity of care when possible—making appointments with providers who are both knowledgeable in the area of incontinence and well acquainted with their particular concerns and circumstances. If self-management techniques fail or incontinence increases, patients should feel comfortable further investigating their symptoms with a familiar provider or continence resource service. As the patient gains confidence in self-monitoring and becomes more proficient at recognizing changes in symptoms, self-efficacy in decision making about resource use is likely to increase.
Developing and implementing an action plan. Once patients have decided on a particular intervention or behavioral change, they need to develop a detailed, realistic action plan. For example, an action plan for practicing pelvic floor muscle exercises might require patients to decide when and where they will perform the exercises, for how long, and in which positions. Nurses should advise their patients to set a feasible timeline for action plan assessment. This may be two to three weeks after a dietary intervention or several months after starting a pelvic floor muscle exercise regimen. If the intervention is unsuccessful, it may be because the self-management behavior was not implemented effectively (for example, the patient may not have performed the exercises correctly or consistently). Evaluation would include assessing whether the patient was able to realistically carry out the action plan and whether any unanticipated events interfered with completion. Action plans may need to be revised to account for unexpected changes in health, work, or family matters, or to include alternative self-management techniques. So patients should be encouraged to review their action plan with the nurse periodically for necessary changes.
Self-monitoring. The ability to self-monitor is a critical component of all self-management strategies. Broadly defined, self-monitoring is an “awareness of symptoms or bodily sensations that is enhanced through periodic measurements, recordings, and observations.”14
Before initiating self-management, patients must become attuned to their symptoms and bodily sensations. Through regular observation and measurement, patients learn to recognize whether a particular intervention or behavioral change produces a positive or negative outcome. For example, patients with urinary incontinence might record the quantity and types of fluids they consume, while tracking the number of times they void daily or the number of “accidents” they have in a week. Patients with fecal incontinence might keep a food diary and record associated fecal leakage so as to identify and limit problem foods in their diet.15,16
Bodily sensations associated with incontinence include bladder or bowel fullness and urgency. Awareness of these sensations can trigger behaviors that address them, and if the behaviors are successful in reducing the associated signs and symptoms, the sensations are more easily recognized the next time they occur.
Setting and attaining goals. Setting realistic goals promotes successful self-management. When patients decide to implement an action plan, nurses can suggest that they set reasonable time frames within which to accomplish specific goals. Nurses can then use a goal-attainment instrument, such as the Self-Assessment Goal Achievement questionnaire, to help patients conduct an honest appraisal of outcomes.17 If goals are met, patients continue with the self-management process; if goals aren't met, patients can either readjust their goals or review the action plan implementation with the nurse. When complete continence isn't possible, alternative goals might include reducing the frequency of incontinence and increasing confidence in self-management.18 If a review of plan implementation reveals barriers, the patient may reformulate the plan or select an alternate treatment modality. Over the long term, symptoms may return or worsen despite adherence to a successful self-management plan. In such cases, the nurse can help the patient investigate possible reasons.
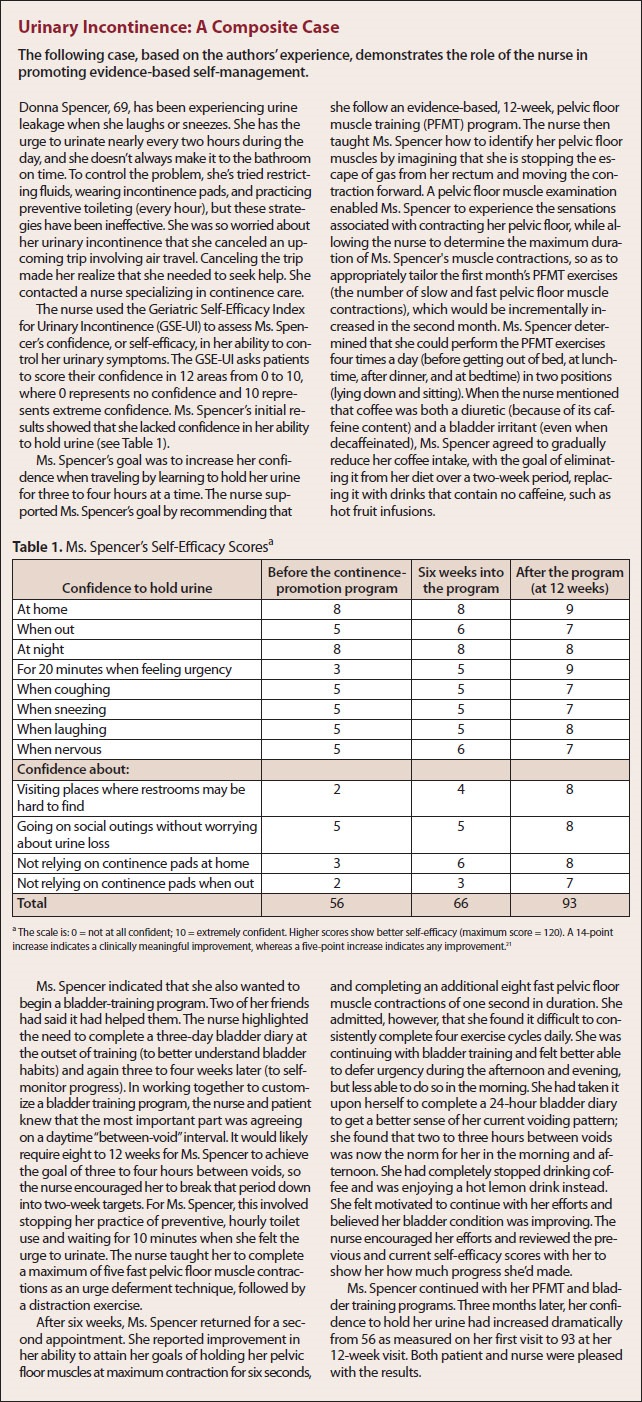
Self-efficacy, which supports self-management behaviors, increases with the development of each. As patients gain confidence in their ability to manage their symptoms, their ability to successfully manage their condition is likely to improve, further motivating them, guiding their actions, and sustaining behavioral changes.19, 20 Nurses can use a self-efficacy scale to measure patients’ confidence.16, 21 For maximum success, self-efficacy measures should be behavior-specific and target each intervention separately.22 For example, in determining the self-efficacy of a patient self-managing urinary incontinence, the nurse would measure the patient's confidence in holding urine when coughing, when sneezing, when laughing, and when nervous within a predetermined time frame after the introduction of each new intervention (see Urinary Incontinence: A Composite Case21).
Urinary Incontinence: A Composite Case
The following strategies may be used to promote self-efficacy in patients 22:
- Point out temporal associations between new skill acquisition and recent successes.
- Reinforce effort and persistence.
- Help identify early symptoms.
- Facilitate peer-modeling opportunities by organizing small discussion groups in which patients who have successfully self-managed incontinence share helpful strategies with others who have similar continence concerns.
- Help struggling patients identify or create meaningful goals.
DELIVERING SUPPORTIVE INTERVENTIONS
There are several means through which to support patients’ self-management behaviors, including
- individualized face-to-face counseling.23-25
- small group sessions.26
- interactive, computer-based continence-promotion systems.27, 28
- informative, paper-based materials.29, 30
Supportive interventions may be delivered in clinics, community centers, or patients’ homes.31 Some research suggests that interactive and collaborative approaches are more successful in supporting self-management for incontinence than passive approaches such as providing standard, written information.
STRATEGIES FOR MANAGING URINARY INCONTINENCE
Research findings and clinical practice support the following interventions for managing urinary incontinence 32-36:
- modifying the amount, type, and timing of fluid intake
- pelvic floor muscle, or Kegel, exercises
- rapid pelvic contraction exercises, often called the “Knack” maneuver
- bladder training, including modifying voiding intervals
- weight management
- constipation management
Modifying fluid intake. Men and women with urinary urgency or incontinence should be advised to avoid caffeinated beverages and not to drink more than their daily fluid requirements. Depending on weight, activity level, climate, and the presence of abnormal fluid loss or such conditions as congestive heart failure or kidney disease, fluid requirements are generally said to be 1,800 to 2,400 mL per day.13, 37
Pelvic floor muscle exercises are designed to strengthen the muscles surrounding the urethra and the external urethral sphincter in order to reduce or prevent urine leakage. The first step is to identify these muscles and to learn how to contract and relax them selectively (without increasing intra-abdominal pressure on the bladder or pelvic floor). The second step is to perform a daily exercise regimen aimed at improving the strength, coordination, and endurance of the muscles. Typically, such a regimen would continue for 12 weeks and would include three sets of a series of 10 sustained pelvic floor muscle contractions, each lasting eight to 10 seconds with a one-to-one or two-to-one relaxation period in between. Nurses may need to remind patients that it takes time to strengthen the pelvic floor muscles and that improvement in urinary incontinence seldom occurs before the exercises have been performed consistently over several weeks. These exercises may be performed while lying down, sitting, or standing.
The “Knack” maneuver calls for patients to remain standing while rapidly contracting their pelvic floor muscles prior to initiating a cough.36 This widely practiced coordination exercise was designed to promote pelvic floor muscle awareness and help patients suppress the feeling of urgency.
Bladder training may be used by cognitively intact and motivated people with urinary incontinence to increase the time interval between voids and to reduce the sensation of urgency. Two main components of bladder training are urge suppression and urge control. Urge suppression involves pausing; sitting down, if possible; relaxing; and contracting the pelvic floor muscles repeatedly in order to diminish the urge to urinate, inhibit detrusor contractions, and prevent urine loss. While waiting for the urge to subside, patients can practice urge control techniques—that is, they can try to distract themselves from the urge to void by focusing instead on a problem-solving challenge or counting backwards from 100 by nines. After the urge to urinate has subsided, patients walk at a normal pace to the toilet. A bladder drill procedure imposes a progressively lengthened interval—from five minutes to four hours, depending on patient tolerance—between voids over the course of days or weeks.
Weight management. Research has shown that women with urinary incontinence who undergo a 5% to 10% weight loss experience tremendous symptom improvement.32 In a multicenter study of nearly 2,000 women with diabetes, weight loss was the lifestyle change that had the greatest positive impact on urinary continence recovery; investigators attributed this finding to the effects of reduced abdominal weight, intra-abdominal pressure, and intravesicular pressure.32
Constipation management. Straining during defecation is significantly associated with such urinary symptoms as detrusor overactivity and urgency.35 This may be a consequence of the rising pressure that straining produces within the abdomen and on the pelvic floor and the pressure that excess fecal mass in the rectum exerts on the bladder, thereby stimulating its stretch receptors and reducing its functional capacity.
STRATEGIES FOR MANAGING FECAL OR DUAL INCONTINENCE
Information collected in a bowel diary can guide self-management interventions for fecal incontinence or dual (fecal with urinary) incontinence. For example, it can help patients schedule appointments, public outings, and exercise routines around anticipated bowel patterns. In addition, it may help patients identify troublesome foods.
Some dietary modifications patients can make to self-manage fecal incontinence include38, 39:
- avoiding greasy and flatus-producing foods, dairy products, fruits with edible seeds (such as strawberries), acidic citrus fruits, nuts, and spicy foods.
- baking or broiling instead of frying.
- eating meals at regular times of the day.
- eating after public events to reduce likelihood of leakage.
Patients who drive often consider driving a self-management strategy, since they can usually leave public events if necessary.40Advise patients to keep a change of underwear and toileting supplies in their car, handbag, briefcase, or backpack, and to wear darker clothing when away from home (so if soiling should occur, it will be less noticeable). Other self-management skills for fecal incontinence include scanning the environment for toilet locations and mapping travel routes with public toilet access.4
Although pelvic floor muscle training is sometimes used for fecal incontinence, it has been less successful in treating fecal than urinary incontinence.41 Strategies for bowel habit training are similar to those used in urinary incontinence, but more research is needed to evaluate their effectiveness.41, 42
Women are more likely than men to wear absorbent pads to manage fecal incontinence.1 Some men prefer to place a small piece of surgical gauze between the buttocks, especially if they tend to have only a small amount of leakage.43
Patients with frequent fecal leakage (occurring daily or several times per week) may take antidiarrheal medication on a daily basis.44 However, since fecal incontinence seldom occurs that frequently, many patients use these medications on an as-needed, preemptory basis—such as before attending a public function.1, 4Men and women with multiple sclerosis report that compared with other self-management strategies, such as using absorbent pads or making dietary modifications, using antidiarrheal medication is the most helpful intervention for controlling fecal incontinence.45
ADDITIONAL INFORMATION
More evidence is needed to establish the effectiveness, costs, optimal duration, and best means of delivering the various interventions that support self-management of urinary and fecal incontinence. As research continues, nurses should consider seeking additional information about supportive interventions; self-management behaviors; the value and safety of “home remedies”; products for managing incontinence from such Web sites as the National Association for Continence (www.NAFC.org), the International Continence Society (www.ICS.org), and the Simon Foundation for Continence (www.simonfoundation.org); incontinence support groups; and other health care providers that work with patients with incontinence.
Mary H. Wilde is an associate professor at the University of Rochester School of Nursing, Rochester, NY.
Donna Z. Bliss is a professor and the School of Nursing foundation professor of research at the University of Minnesota, Minneapolis. Joanne Booth is a reader/research coordinator in the School of Health and Life Sciences at Glasgow Caledonian University, Glasgow, Scotland, United Kingdom.
Francine M. Cheater is a professor and director of research in the School of Nursing Sciences, Faculty of Medicine and Health Sciences, at the University of East Anglia, Norwich, England, United Kingdom.
Cara Tannenbaum is an associate professor of medicine at the Université de Montréal and director of the Geriatric Incontinence Clinic at the Institut Universitaire de Gériatrie de Montréal, Quebec, Canada.
The authors and planners have disclosed no potential conflicts of interest, financial or otherwise.
REFERENCES
1. Bliss DZ, et al. Managing fecal incontinence: self-care practices of older adults. J Gerontol Nurs 2005;31(7):35-44.
2. Horrocks S, et al. What prevents older people from seeking treatment for urinary incontinence? A qualitative exploration of barriers to the use of community continence services. Fam Pract 2004;21(6):689-96.
3. Shaw C, et al. Barriers to help seeking in people with urinary symptoms. Fam Pract 2001;18(1):48-52.
4. Peden-McAlpine C, et al. The experience of communityliving women managing fecal incontinence. West J Nurs Res 2008;30(7):817-35. 5. Bodenheimer T, et al. Patient self-management of chronic disease in primary care. JAMA 2002;288(19):2469-75. 6. Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26(1):1-7.
7. Richard AA, Shea K. Delineation of self-care and associated concepts. J Nurs Scholarsh 2011;43(3):255-64. 8. Schulman-Green D, et al. Processes of self-management in chronic illness. J Nurs Scholarsh 2012;44(2):136-44. 9. Riegel B, et al. A middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci 2012;35(3):194-204.
10. Thorne SE, et al. Attitudes toward patient expertise in chronic illness. Int J Nurs Stud 2000;37(4):303-11.
11. Wilkinson A, Whitehead L. Evolution of the concept of selfcare and implications for nurses: a literature review. Int J Nurs Stud 2009;46(8):1143-7.
12. Abrams P, et al., eds. Incontinence: 5th international consultation on incontinence. 5th ed. Arnheim, The Netherlands: European Association of Urology; 2013.
13. Gray M, Krissovich M. Does fluid intake influence the risk for urinary incontinence, urinary tract infection, and bladder cancer? J Wound Ostomy Continence Nurs 2003;30(3): 126-31.
14. Wilde MH, Garvin S. A concept analysis of self-monitoring. J Adv Nurs 2007;57(3):339-50.
15. Fisher K, et al. Comparison of recall and daily self-report of fecal incontinence severity. J Wound Ostomy Continence Nurs 2008;35(5):515-20.
16. Tannenbaum C, et al. Creation and testing of the Geriatric Self-Efficacy Index for Urinary Incontinence. J Am Geriatr Soc 2008;56(3):542-7.
17. Brubaker L, et al. Goal attainment scaling in patients with lower urinary tract symptoms: development and pilot testing of the Self-Assessment Goal Achievement (SAGA) questionnaire. Int Urogynecol J 2011;22(8):937-46.
18. Manthey A, et al. Goals of fecal incontinence management identified by community-living incontinent adults. West J Nurs Res 2010;32(5):644-61.
19. Wilson M. The impact of faecal incontinence on the quality of life. Br J Nurs 2007;16(4):204-7.
20. Wilson M, McColl E. The experience of living with faecal incontinence. Nurs Times 2007;103(14):46-9.
21. Tannenbaum C, et al. Responsiveness and clinical utility of the Geriatric Self-Efficacy Index for Urinary Incontinence. J Am Geriatr Soc 2009;57(3):470-5.
22. Bandura A. Self-efficacy: the exercise of control. New York: W.H. Freeman; 1997.
23. Kincade JE, et al. Randomized clinical trial of efficacy of self-monitoring techniques to treat urinary incontinence in women. Neurourol Urodyn 2007;26(4):507-11.
24. Wagg AR, et al. A randomised partially controlled trial to assess the impact of self-help vs. structured help from a continence nurse specialist in women with undiagnosed urinary problems in primary care. Int J Clin Pract 2007;61(11): 1863-73.
25. Williams KS, et al. A randomized controlled trial of the effectiveness of pelvic floor therapies for urodynamic stress and mixed incontinence. BJU Int 2006;98(5):1043-50.
26. McFall SL, et al. Outcomes of a small group educational intervention for urinary incontinence: health-related quality of life. J Aging Health 2000;12(3):301-17.
27. Boyington AR, et al. Effectiveness of a computer-based system to deliver a continence health promotion intervention. J Wound Ostomy Continence Nurs 2005;32(4):246-54.
28. Ruiz JG, et al. Development and pilot testing of a selfmanagement Internet-based program for older adults with overactive bladder. Urology 2011;78(1):48-53.
29. Franzen K, et al. Urinary incontinence: Evaluation of an information campaign directed towards the general public. Scand J Urol Nephrol 2008;42(6):534-8.
30. Holroyd-Leduc JM, et al. Translation of evidence into a selfmanagement tool for use by women with urinary incontinence. Age Ageing 2011;40(2):227-33.
31. Wolters R, et al. Effects of distance learning on clinical management of LUTS in primary care: a randomised trial. Patient Educ Couns 2005;59(2):212-8.
32. Brown JS, et al. Lifestyle intervention is associated with lower prevalence of urinary incontinence: the Diabetes Prevention Program. Diabetes Care 2006;29(2):385-90.
33. Hay Smith J, et al. Adult conservative management. In: Abrams P, et al., eds. Incontinence: 4th international consultation on incontinence. 4th ed. London: Health Publications Ltd; 2009. p. 1025-120. http://www.icud.info/PDFs/Incontinence.pdf.
34. Hay-Smith EJ, et al. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev 2011(12):CD009508.
35. Kaplan SA, et al. Systematic review of the relationship between bladder and bowel function: implications for patient management. Int J Clin Pract 2013;67(3):205-16.
36. Miller JM, et al. Clarification and confirmation of the Knack maneuver: the effect of volitional pelvic floor muscle contraction to preempt expected stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 2008;19(6):773-82.
37. Burgio KL. Behavioral treatment of urinary incontinence, voiding dysfunction, and overactive bladder. Obstet Gynecol Clin North Am 2009;36(3):475-91.
38. Croswell E, et al. Diet and eating pattern modifications used by community-living adults to manage their fecal incontinence. J Wound Ostomy Continence Nurs 2010;37(6):677-82.
39. Hansen JL, et al. Diet strategies used by women to manage fecal incontinence. J Wound Ostomy Continence Nurs 2006;33(1):52-61.
40. Collings S, Norton C. Women’s experiences of faecal incontinence: a study. Br J Community Nurs 2004;9(12):520-3.
41. Norton C, et al. Conservative and pharmacological management of faecal incontinence in adults. In: Abrams P, et al., eds. Incontinence: 4th international consultation on incontinence. 4th ed. London: Health Publications Ltd; 2009. p. 1321-86. http://www.icud.info/PDFs/Incontinence.pdf.
42. Bliss DZ, Norton C. Conservative management of fecal incontinence. Am J Nurs 2010;110(9):30-8.
43. Bliss DZ, Savik K. Use of an absorbent dressing specifically for fecal incontinence. J Wound Ostomy Continence Nurs 2008;35(2):221-8.
44. Bliss DZ, et al. Assessment and conservative management of faecal incontinence and quality of life in adults. In: Abrams P, et al., eds. Incontinence: 5th international consultation on incontinence. Arnheim, The Netherlands: European Association of Urology; 2013. p. 1443-85.
45. Norton C, Chelvanayagam S. Bowel problems and coping strategies in people with multiple sclerosis. Br J Nurs 2010; 19(4):220-6.
