Physical and Cognitive Functions, Physical Activity, and Sedentary Behavior in Older Adults With Multiple Sclerosis
Why is this study important?
As our population ages and new disease-modifying therapies come to market, the number of older individuals with MS will likely continue to grow. Aging brings some changes in physical and cognitive function in people whether they have MS or not. For people with MS, aging brings with it problems that likely add to the effects of MS, so that people growing older with MS may experience challenges in their cognitive and physical functions that are greater than those of people who do not have MS.
The authors were familiar with a 2016 study suggesting that older (i.e., people 60 years of age and older) people with MS spend more time being sedentary and are less likely to engage in moderate-to-vigorous physical activity than younger and middle-aged people with MS. This observation begs an interesting question: does sedentary behavior and lack of physical activity in older individuals with MS contribute to increased physical and cognitive challenges? If this is true, then is the reverse also true? That is, can engaging in more frequent moderate-to-vigorous physical activity and reducing sedentary behavior limit or delay decline in physical and cognitive function?
This study takes a first step in understanding the relationship between physical and cognitive function and physical activity in older individuals with MS.
How did the authors carry out their study?
The investigators recruited 40 older individuals with MS. For the most part, these individuals had RRMS, and the mean time following their diagnosis was more than 20 years. They had all been relapse-free for at least one month, and they were able to walk with or without assistance. The researchers then recruited 40 older people who did not have MS and were also able to walk with or without some assistance. The mean ages of the two groups were fairly similar: 65.3 years in the MS group, and 66.5 years in the non-MS group.
The individuals in the study participated in a series of tests to evaluate their cognitive levels, followed by tests to assess their physical function. Each participant was then asked to wear an accelerometer and keep a log book of their wearing time for 7 days.
What did the results show?
A great deal of this article is devoted to statistical analysis of their assessments: unless you are particularly fond of such, you may want to jump to the “Discussion” section, because the results are fascinating:
- Are older people with MS more likely to be sedentary than their counterparts? Yes, the authors noted that older people with MS “engaged in less MVPA [Moderate-to-Vigorous Physical Activity], more sedentary behavior, and longer duration of long (≥ 30 minutes) sedentary bouts” than participants who did not have MS.
- Did these older individuals with MS appear to have reduced physical function than their counterparts? Yes: in all measurements of physical function, older people with MS had greater impairment than their counterparts without MS.
- Do older people with MS experience inferior cognitive function compared to older individuals without MS? Not really – the results suggest that only in one area — information-processing speed — did older people with MS perform less well than individuals who did not have MS.
But here’s the particularly interesting part: At least part of the differences in impairment between the participants with MS and those without MS could be attributed to less physical activity and more sedentary behavior in the group with MS. The authors noted that the intensity of activity and the frequency of that activity appear to make a significant difference in maintaining physical function in older adults with MS.
How does one know if their physical activity qualifies as “moderate to vigorous”? The intensity of physical activity is important if one is to benefit from it: a leisurely stroll around the kitchen will probably not cut it for most people. This is where a physical therapist or personal trainer may be able to help both in identifying the level of activity most likely reap beneficial effects as well as to plan an activity program that meets your needs. Ask your healthcare provider to help you connect with resources in your area.
Keep in mind
All studies such as this have some limitations. The authors listed these limitations about their study:
- This is a study of correlation not cause: that is, the investigators point out that, although there appears to be a relationship between low levels of physical activity and reduced physical function, this study does not demonstrate that one causes the other
- The study results may not apply to individuals with MS who are older than 70
- The individuals with MS in the study had mild-to-moderate levels of disability: these study results may not apply to individuals with greater levels of disability
- The study does not take in account the role of fatigue in influencing the frequency and intensity of older adults with MS.
Original Article
Physical and Cognitive Functions, Physical Activity, and Sedentary Behavior in Older Adults With Multiple Sclerosis
Rachel E. Bollaert, PhD; Robert W. Motl, PhD
Journal of Geriatric Physical Therapy
Background and Purpose: Older adults with multiple sclerosis (MS) experience age-related declines in physical and cognitive functions that may be compounded by the disease and its progression and worsened by physical inactivity and sedentary behavior. However, the extent to which impairments in physical and cognitive functions are manifestations of MS and disease progression, reflective of the general aging process, or perhaps 2 detrimental processes exacerbating the synergistic effects of the other is relatively unknown. This study compared physical and cognitive functions, sedentary behavior, and physical activity between 40 older adults with MS (ie, 60 years of age and older) and 40 age- and sex-matched healthy older adults. We further examined whether physical activity and/or sedentary behavior explained differences between groups in physical and cognitive functions.
Methods: Participants initially underwent the cognitive assessments, followed by the physical function assessments. The order of tests was standardized and participants were provided seated-rest between the administrations of the physical function assessments. Participants were then instructed to wear an accelerometer and document wear time in a log book for a 7-day period after the testing session.
Results: Multivariate analyses of variance indicated that older adults with MS (n = 40) performed worse on all measures of physical function, and 1 measure of cognitive function (ie, information-processing speed), compared with healthy controls (n = 40). Older adults with MS engaged in less moderate-to-vigorous physical activity, more sedentary behavior, and longer duration of long sedentary bouts than healthy controls. Pearson correlations demonstrated that levels and patterns of physical activity were significantly associated with a majority of physical function variables but not cognitive function variables in both older adults with MS and healthy controls but to a greater extent in older adults with MS. Partial Pearson correlations further demonstrated that levels and patterns of sedentary behavior were significantly associated with a majority of physical function variables but not cognitive function variables primarily in older adults with MS. Linear regression analyses indicated that levels and patterns of physical activity and sedentary behavior partially accounted for differences in physical and cognitive function variables between older adults with MS and healthy controls.
Conclusion: There is evidence of reduced function in older adults with MS, and this might be partially managed by behavioral interventions that target physical activity and sedentary behavior for the promotion of healthy aging in older adults with MS.
Introduction
There is a shift in the aging demography of multiple sclerosis (MS), such that there are more older adults with MS than ever before. This portends considerable public health impact for society and clinical burden for health care providers based on putative declines in physical and cognitive functions and associated changes in physical activity and sedentary behaviors.1,2 The increasing population of older adults with MS likely undergoes age-related declines in physical and cognitive functions that are superimposed on those associated with the disease itself and its progression.3–7 This suggests that living an additional 20 years with MS, for example, might reduce function above and beyond the effect of normal declines associated with aging alone.
There is additional evidence for changes in physical activity and sedentary behavior in older adults with MS.8 One study demonstrated that older adults with MS engaged in significantly less moderate-to-vigorous physical activity (MVPA) and more sedentary behavior per day than young and middle-aged adults with MS.8 To that end, a focus on physical activity and sedentary behaviors in older adults with MS is important, as changing these behaviors may represent a novel approach for healthy aging with MS.9,10 This is necessary as very little is known about managing the consequences of MS in older adults.3,11 Physical activity may provide a protective or potentially restorative effect on the mechanisms associated with aging and MS that influence physical and cognitive functions.10,12,13
The current study compared physical and cognitive functions between older adults with MS (ie, 60 years of age and older) and age- and sex-matched healthy older adults from the general population and examined the possibility that rates and patterns of objectively measured physical activity and sedentary behavior explained the differences in these functions between groups.
Methods
Participants
The sample included 40 older adults with MS and 40 age- and sex-matched healthy controls 60 years of age and older. These participants were recruited from April 2016 to February 2017 from a mailing list of persons with MS in Illinois, a database of previous research volunteers, and a research advertisement posted on the Web site of the Greater Illinois chapter of the National Multiple Sclerosis Society. The healthy controls were recruited through a campus-wide, e-mail listserv. Participants were screened via telephone with the inclusion criteria for older adults with MS as 60 years of age and older; diagnosis of MS; relapse free in the last 30 days; ambulatory with or without assistance; and willing and able to visit the laboratory for 1 testing session. The inclusion criteria for the healthy controls were the same except for the diagnosis of MS and relapse free in the last 30 days.
Measures
Physical function
The Timed 25-Foot Walk (T25FW) was administrated as a measure of walking speed14; the Six-Minute Walk (6MW) as a measure of walking endurance15; the Timed Up-and-Go (TUG) as a measure of functional mobility16; the Six-Spot Step Test (6SST) as a measure of ambulatory function17; and the Short Physical Performance Battery (SPPB) as a measure of lower extremity function including standing balance, gait speed, and chair rises.5
Cognitive function
The Symbol Digit Modalities Test (SDMT)18 and Paced Auditory Serial Addition Test19 were included as measures of information processing speed; the California Verbal Learning Test-II20 as a measure of verbal learning and memory; and the Brief Visuospatial Memory Test-Revised21 as a measure of visual learning and memory.
Sedentary behavior and physical activity
Sedentary behavior and physical activity were objectively measured with ActiGraph GT3X+ accelerometers (Health One Technology, Fort Walton Beach, Florida). The raw activity data were downloaded using software (ActiLife 8) and the data were processed for daily accelerometer wear time (minutes) and time spent in sedentary behavior (≤99 counts per minute), light physical activity (LPA) (100-1722 counts per minute), and MVPA (≥1723 counts/minute) for older adults with MS and time spent in sedentary behavior (≤99 counts per minute), LPA (100-2016 counts per minute), and MVPA (≥2017 counts per minute) for healthy controls.22 The LPA, MVPA, and sedentary behavior are reported as both minutes per day and as percentage of daily wear time, as it accounts for variation in wear time among participants. Accelerometry further provided data on patterns of sedentary behavior and physical activity including number and average duration (minutes) of sedentary bouts; long sedentary bouts (>30 minutes); and activity bouts.23 In the overall sample, all participants had 4 or more days of valid accelerometer data.24
Disability status
All older adults with MS underwent a neurological examination by a neurostatus-certified examiner to generate Expanded Disability Status Scale scores25 for describing the disability status of the sample.
Procedure
The procedure was approved by the Institutional Review Board at the University of Illinois Urbana-Champaign, and all participants provided written informed consent before participating in study procedures. From the months of April 2016 through February 2017, participants underwent a neurological examination and the cognitive and physical function assessments in a university laboratory and wore the accelerometer for a 7-day period.
Data Analysis
Data were analyzed in SPSS Statistics Version 24 (IBM Corporation, Armonk, New York) in March 2017. We examined group differences (ie, older adults with MS vs controls) in sets of physical and cognitive function variables and physical activity and sedentary behavior variables using multivariate analysis of variance (MANOVA). We examined the overall F test and Wilks' Lambda (λ) for identifying an overall, statistically significant multivariate main effect for group on sets of outcomes. We inspected the resulting univariate analyses of variance (ANOVAs) for identifying specific group differences in outcomes per set. We compared the effects across ANOVAs using partial eta-squared (ηp2) with values of 0.04, 0.06, and 0.09 representing small, moderate, or strong effects, respectively,26 and reported the magnitude of group differences in mean scores using Cohen d with values of 0.2, 0.5, and 0.8 representing small, moderate, and large differences, respectively.27 Pearson product-moment correlations (r) were calculated among physical and cognitive function variables, physical activity, and sedentary behavior for the entire sample and subsamples of older adults with MS and healthy controls. Values for correlation coefficients of 0.1, 0.3, and 0.5 were interpreted as weak, moderate, and strong, respectively.27 We further examined whether physical activity and/or sedentary behavior accounted for differences in physical and cognitive functions between older adults with MS and healthy controls using stepwise linear regression analysis. This was undertaken by regressing physical and/or cognitive function variables on group in step 1 and then adding physical activity and sedentary behavior variables in step 2. The β-coefficients for the effect of group on physical and cognitive function variables were compared between step 1 and step 2 to examine whether physical activity and/or sedentary behavior accounted for the differences between group.
Results
Participant Characteristics
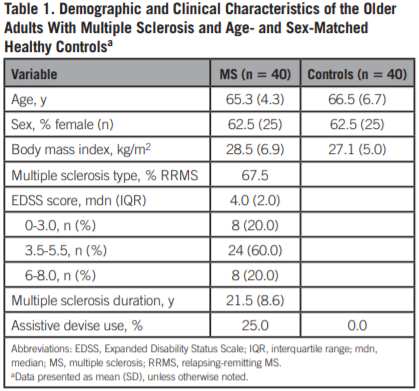
Demographic and clinical characteristics of the samples are presented in Table 1. Briefly, the mean (SD) age for older adults with MS and healthy controls were similar [65.3 (4.3) and 66.5 (6.7), respectively]. Older adults with MS had predominantly relapsing-remitting MS, a mean (SD) disease duration of 21.5 (8.6) years, and moderate disability based on the median Expanded Disability Status Scale score (4.0 [interquartile range = 2.0]).
Physical and Cognitive Function, Accelerometry, Physical Activity, and Sedentary Behavior
Descriptive data and statistical analyses of physical and cognitive functions, physical activity, and sedentary behavior for older adults with MS and age- and sex-matched healthy controls are presented in Table 2.
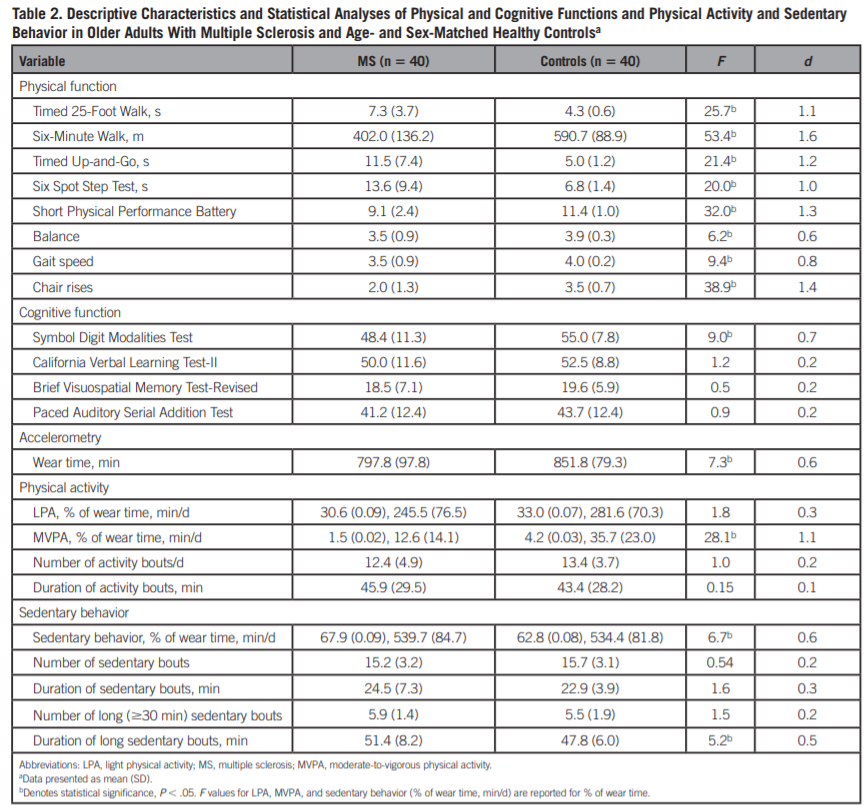
Physical function
The MANOVA identified a significant multivariate main effect for group (ie, older adults with MS vs controls) (Wilks' λ= 0.555, F7,71 = 8.12; P < .001, ηp2 = 0.445). Significant and large univariate main effects were obtained for T25FW (F1,77 = 25.71; P < .001, d = 1.1); 6MW (F1,77 = 53.43; P < .001, d = 1.6); TUG (F1,77 = 21.38; P < .001, d = 1.2); 6SST (F1,77 = 20.00; P < .001, d = 1.0); and total SPPB score (F1,77 = 32.01; P < .001, d = 1.3). There were significant and large univariate main effects for the gait speed (F1,77 = 9.36; P < .005, d = 0.8) and chair rises components (F1,77 = 38.90; P < .001, d = 1.4) of the SPPB, and a moderate difference for the balance component of the SPPB (F1,77 = 6.23; P < .05, d = 0.6).
Cognitive function
The MANOVA did not reveal a significant multivariate main effect for group (Wilks' λ= 0.892, F4,74 = 2.23; P = .07, ηp2 = 0.108). When examining the univariate main effects, a significant univariate main effect with a moderate difference in magnitude was obtained for SDMT (F1,77 = 8.96; P < .005, d = 0.7). [Editor's Note: When the overall multivariate statistic is not significant, subsequent univariate findings of significance are typically not reported as the multivariate error rate is not adequately controlled.]
Physical activity
The MANOVA revealed a significant multivariate main effect for group (Wilks' λ= 0.723, F4,74 = 7.10; P < .001, ηp2 = 0.277). There was a significant and large univariate main effect for MVPA (F1,77 = 28.08; P < .001, d = 1.1).
Sedentary behavior
The MANOVA revealed a significant multivariate main effect for group (Wilks' λ= 0.818, F5,73 = 3.24; P < .015, ηp2 = 0.182). Significant univariate main effects with moderate differences in magnitude were obtained for sedentary behavior (F1,77 = 6.737; P < .015, d = 0.6) and the duration of long sedentary bouts (≥30 minutes) (F1,77 = 5.165; P < .05, d = 0.5).
Physical Activity and Physical and Cognitive Function
The associations among physical and cognitive functions and physical activity in the separate and combined samples of older adults with MS and age- and sex-matched healthy controls are presented in Table 3.
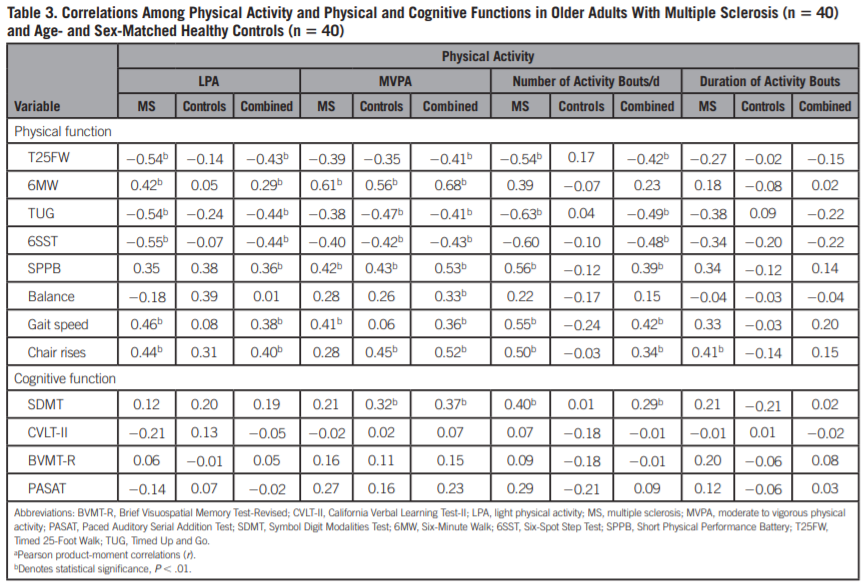
Physical function
In the combined sample, the Pearson correlations (r) indicated statistically significant (P < .01) and small-to-moderate associations between LPA and number of activity bouts per day and most physical function variables. There were statistically significant and moderate-to-large associations between MVPA and all physical function variables.
In older adults with MS, the Pearson correlations (r) indicated statistically significant and moderate-to-large associations between LPA and number of activity bouts per day and most physical function variables. There were moderate-to-large associations between MVPA and duration of activity bouts and very few physical function variables in older adults with MS. In healthy controls, there were statistically significant and moderate-to-large associations between MVPA and most physical function variables.
Cognitive function
There were statistically significant (P < .01) and small-to-moderate associations in the combined sample between MVPA and SDMT and number of activity bouts per day and SDMT. There were further significant and moderate associations between SDMT and number of activity bouts per day in older adults with MS and MVPA in controls.
Sedentary Behavior and Physical and Cognitive Function
The associations among physical and cognitive functions and sedentary behavior in the separate and combined samples of older adults with MS and age- and sex-matched healthy controls are presented in Table 4.
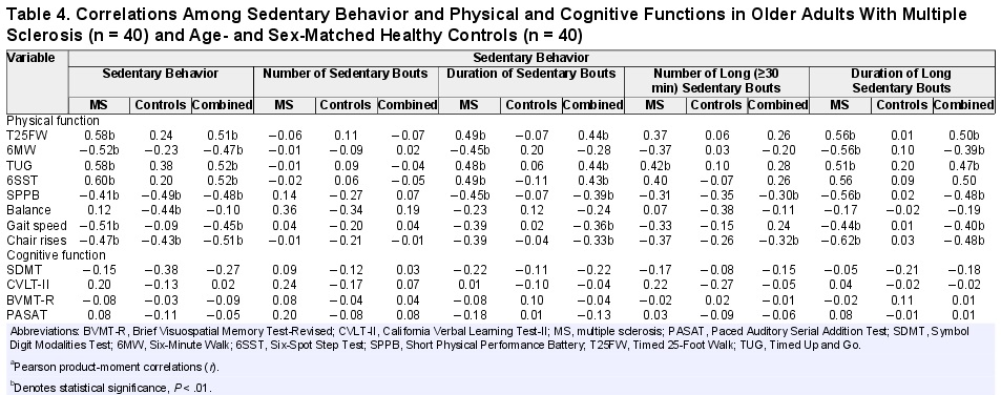
Physical function
In the combined sample, the Pearson correlations (r) indicated statistically significant (P < .01) moderate-to-large associations between sedentary behavior and the duration of sedentary bouts and long sedentary bouts and most physical function variables. There were few moderate associations between the number of long (≥30 minutes) sedentary bouts and physical function variables and no associations for the number of sedentary bouts.
In older adults with MS, the Pearson correlations (r) indicated statistically significant and moderate-to-large associations between sedentary behavior, duration of sedentary bouts and of long (≥30 minutes) sedentary bouts, and most physical function variables. There was 1 moderate association between TUG and number of long (≥30 minutes) sedentary bouts and no associations for number of sedentary bouts. In healthy controls, the only statistically significant and moderate associations were between sedentary behavior and few physical function variables.
Cognitive function
There were no statistically significant associations between any of the sedentary behavior variables and cognitive function variables in the combined sample, older adults with MS, or controls.
Linear Regression
The stepwise linear regression analyses are presented in Table 5. All physical and cognitive function variables that significantly differed between groups (ie, older adults with MS vs healthy controls) and that correlated across groups were included in this analysis.
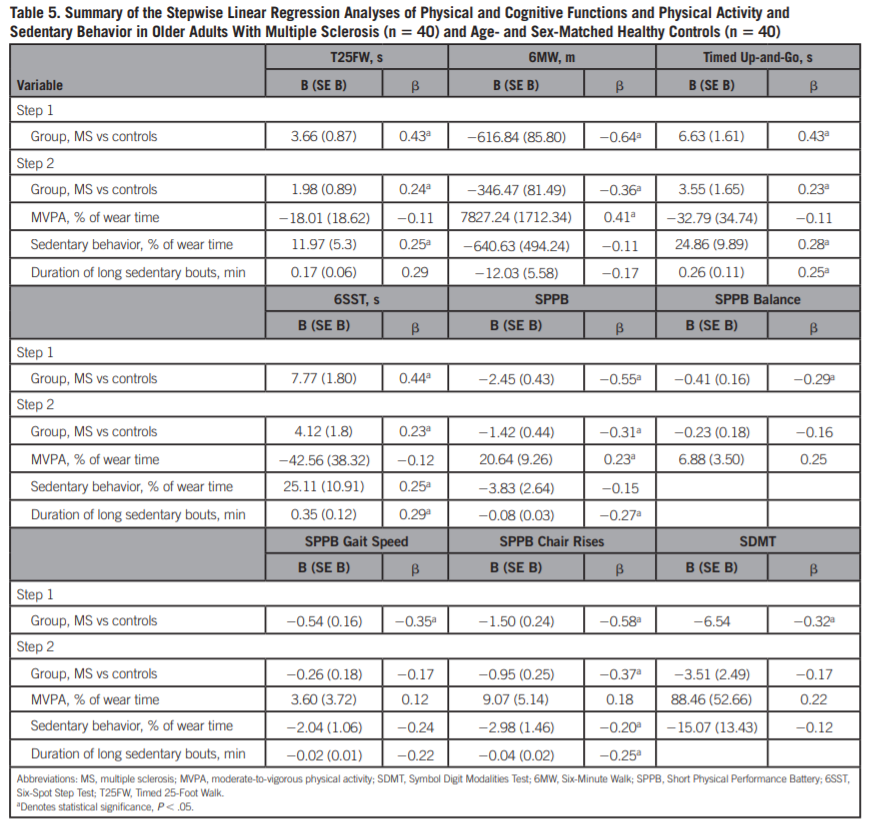
Physical function
Briefly, when the T25FW, 6MW, TUG, 6SST, total SPPB score, and chair rises subcomponent of the SPPB were regressed on group in step 1, the β-coefficients were statistically significant; when MVPA, sedentary behavior, and the duration of long (≥30 minutes) sedentary bouts were added in step 2, the β-coefficient become attenuated but was still significant. When the balance and gait speed components of the SPPB were regressed on group in step 1, the β-coefficients were statistically significant; when MVPA, sedentary behavior, and the duration of long (≥30 minutes) sedentary bouts were added in step 2, the β-coefficients became attenuated and no longer statistically significant.
Cognitive function
When the SDMT was regressed on group in step 1, the β-coefficient was statistically significant; when MVPA, sedentary behavior, and the duration of long (≥30 minutes) sedentary bouts were added in step 2, the β-coefficient became attenuated and no longer statistically significant.
Discussion
The current study compared physical and cognitive functions between older adults with MS (ie, 60 years of age and older) and age- and sex-matched healthy older adults in the general population and examined the possibility that rates and patterns of objectively measured physical activity and sedentary behavior explained the differences in these functions between groups. The primary results of the present study were as follows: (a) older adults with MS demonstrated greater impairments in all measures of physical function and 1 measure of cognitive function than healthy controls; (b) older adults with MS engaged in less MVPA, more sedentary behavior, and longer duration of long (≥30 minutes) sedentary bouts than healthy controls; (c) physical activity, specifically LPA and MVPA, and the number of activity bouts per day were significantly associated with a majority of physical function variables in both older adults with MS and healthy controls but to a greater extent in older adults with MS; (d) sedentary behavior, specifically minutes per day of sedentary behavior, duration of sedentary bouts, and the number and duration of long sedentary bouts were significantly associated with a majority of physical function variables primarily in older adults with MS; and (e) both levels of MVPA and sedentary behavior and patterns of sedentary behavior (ie, duration of long sedentary bouts) partially explained the differences in physical and cognitive functions between older adults with MS and healthy controls.
All measures of physical function demonstrated either moderate or large differences between older adults and healthy controls based on effect size (d). Regarding the T25FW, older adults with MS completed the assessment in 7.3 (3.7) seconds-previous research has demonstrated that a T25FW time of 6.0 to 7.99 seconds is associated with occupational disability and needing “some help” with instrumental activities of daily living in middle-aged adults with MS.28 Furthermore, the mean total SPPB score of 9.1 in the current sample of older adults with MS was below the cutoff value of 10.0, indicating elevated risk for developing future disability.29 Older adults with MS only performed worse in 1 measure of cognitive function (ie, SDMT) compared with healthy controls (48.4 (11.3) and 55.0 (7.8), respectively). These results suggest that older adults with MS may be at a higher risk of motor dysfunction than cognitive dysfunction. Our results supplement a recent study that demonstrated that aging process may affect physical and cognitive functions differently in persons with MS.7,30 Previous research has identified hypotheses for this discrepancy in worsened physical and cognitive functions in older adults with MS, such as pathological changes specifically impacting physical function as well as the influence of cognitive reserve7; however, the underlying cause is still ambiguous. This result warrants the need for future research to further examine this discrepancy, including studies on brain structure and function using magnetic resonance imaging.
Importantly, levels of MVPA and sedentary behavior, as well as patterns of sedentary behavior (ie, duration of long sedentary bouts), might partially influence the magnitude of differences in both physical and cognitive functions between older adults with MS and healthy controls. Older adults with MS engaged in less MVPA and more sedentary behavior and longer duration of long (≥30 minutes) sedentary bouts than healthy controls. Physical activity, specifically LPA and MVPA, and the number of activity bouts per day were significantly associated with most physical function variables in the combined samples of older adults with MS and healthy controls but to a greater extent in older adults with MS. Importantly, the many beneficial effects of physical activity are very much dependent on intensity and this highlights the need for behavioral interventions, as well as physical therapists or personal trainers, to focus on increasing MVPA in older adults with MS. Regarding the cognitive function variables, there were very few associations with physical function variables in both groups. Sedentary behavior, specifically levels of sedentary behavior per day, the duration of sedentary bouts, and the duration of long sedentary bouts were significantly associated with many physical function variables but not cognitive function variables primarily in older adults with MS. The current study is novel in that patterns of sedentary behavior were also moderately associated with physical function and support the notion that transitions from sedentary to nonsedentary behavior are important for physical function in addition to cardiometabolic health.31
The current study involved a relatively large sample size, direct comparisons of older adults with MS and age- and sex-matched healthy controls, and objective and comprehensive measurements of sedentary behavior, physical activity, and physical and cognitive functions. However, there are several limitations. First, this study utilized a cross-sectional research design and, therefore, the results of this study suggest only correlations among sedentary behavior, physical activity, and function but no determination of causation. Future longitudinal research is warranted to further examine these causal associations. The current sample of older adults with MS and healthy controls were relatively young and perhaps the results may not be fully generalized to adults older than 65 to 70 years. Furthermore, the majority of the sample of older adults with MS had mild to moderate disability (ie, Expanded Disability Status Scale score of 3.5-5.5; 60%), and, therefore, the current results may also not be generalized to older adults with higher levels of disability. Finally, the current study did not include other measures that may have affected the associations of sedentary behavior, physical activity, and physical and cognitive functions, such as fatigue, which are highly prevalent in persons with MS.32
Conclusion
In conclusion, the current study demonstrated that older adults with MS (ie, 60 years of age and older) had greater deficits in many areas of physical function (ie, walking speed and endurance and lower extremity strength) but only 1 area of cognitive function (ie, information-processing speed) than age- and sex-matched healthy controls. Older adults with MS further engaged in lower levels of MVPA, higher levels of sedentary behavior, and longer duration of long (≥30 minutes) sedentary bouts than healthy controls. Both levels and patterns of physical activity and sedentary behavior were associated with physical function to a greater extent in older adults with MS than in healthy controls. Importantly, the low levels of MVPA, higher levels of sedentary behavior, and longer duration of long sedentary bouts in older adults with MS partially contributed to the differences in physical and cognitive functions. Overall, such results identify a large decline in physical function but not cognitive function in older adults with MS compared with healthy controls, and that both levels and patterns of physical activity and sedentary behavior should be an emphasis of clinical rehabilitation and behavioral interventions for the promotion of healthy aging in older adults with MS.
References
1. Marrie RA, Yu N, Blanchard J, Leung S, Elliott L. The rising prevalence and changing age distribution of multiple sclerosis in Manitoba. Neurology. 2010;74(6):465–471.
2. Hurwitz BJ. Analysis of current multiple sclerosis registries. Neurology. 2011;76(suppl 1):S7–S13.
3. Awad A, Stüve O. Multiple sclerosis in the elderly patient. Drugs Aging. 2010;27(4):283–294.
4. Stern M, Sorkin L, Milton K, Sperber K. Aging with multiple sclerosis. Phys Med Rehabil Clin N Am. 2010;21(2):403–417.
5. Motl RW, Learmonth YC, Wójcicki TR, et al Preliminary validation of the Short Physical Performance Battery in older adults with multiple sclerosis: secondary data analysis. BMC Geriatr. 2015;15:157.
6. Motl RW, Chaparro G, Hernandez ME, Balto JM, Sandroff BM. Physical function in older adults with multiple sclerosis: an application of the Short Physical Performance Battery. J Geriatr Phys Ther. 2018;41(3):155–160.
7. Roy S, Frndak S, Drake AS, et al Differential effects of aging on motor and cognitive functioning in multiple sclerosis. Mult Scler. 2017;23(10):1385–1393.
8. Klaren RE, Sebastiao E, Chiu CY, Kinnett-Hopkins D, McAuley E, Motl RW. Levels and rates of physical activity in older adults with multiple sclerosis. Aging Dis. 2016;7(3):278–284.
9. Sanai SA, Saini V, Benedict RH, et al Aging and multiple sclerosis. Mult Scler. 2016;22(6):717–725.
10. Motl RW, Sebastiao E, Klaren RE, McAuley E, Stine-Morrow EAL, Roberts B. Physical activity and healthy aging with multiple sclerosis—literature review and research directions. US Neurol. 2016;12(1):29–33.
11. Shirani A, Zhao Y, Petkau J, et al Multiple sclerosis in older adults: the clinical profile and impact of interferon beta treatment. Biomed Res Int. 2015;2015:451912.
12. Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? A critical review of the scientific evidence. Am J Prev Med. 2003;25(3 suppl 2):129–136.
13. Motl RW, Sandroff BM. Benefits of exercise training in multiple sclerosis. Curr Neurol Neurosci Rep. 2015;15(9):62.
14. Kiesseier B, Pozzilli C. Assessing walking disability in multiple sclerosis. Mult Scler. 2012;18(7):914–924.
15. Goldman MD, Marrie RA, Cohen JA. Evaluation of the Six-Minute Walk in multiple sclerosis subjects and healthy controls. Mult Scler. 2008;14(3):383–390.
16. Sebastiao E, Sandroff BM, Learmonth YC, Motl RW. Validity of the Timed Up and Go Test as a measure of functional mobility in persons with multiple sclerosis. Arch Phys Med Rehabil. 2015;97(7):1072–1077.
17. Sandroff BM, Motl RW, Sosnoff JJ, Pula JH. Further validation of the Six-Spot Step Test as a measure of ambulation in multiple sclerosis. Gait Posture. 2015;41(1):222–227.
18. Smith A. Symbol Digit Modalities Test: Manual. Los Angeles, CA: Western Psychological Services; 1982.
19. Fischer JS, Rudick RA, Cutter GR, Reingold SC. The Multiple Sclerosis Functional Composite Measure (MSFC): an integrated approach to MS clinical outcome assessment. National MS Society Clinical Outcomes Assessment Task Force. Mult Scler. 1999;5(4):244–250.
20. Delis DC, Kramer JH, Kaplan E, Ober BA. California Verbal Learning Test (CVLT-II). 2nd ed. San Antonio, TX: Psychological Corporation; 2000.
21. Benedict RH. The Brief Visuospatial Memory Test Revised (BVMT-R). Lutz, FL: Psychosocial Assessment Resources Inc; 1997.
22. Sandroff BM, Motl RW, Suh Y. Accelerometer output and its association with energy expenditure in persons with multiple sclerosis. J Rehabil Res Dev. 2012;49(3):467–475.
23. Ezeugwu V, Klaren RE, Hubbard EA, Manns P, Motl RW. Mobility disability and the pattern of accelerometer-derived sedentary and physical activity behaviors in people with multiple sclerosis. Prev Med Rep. 2015;2:241–246.
24. Motl RW, Zhu W, Park Y, McAuley E, Scott JA, Snook EM. Reliability of scores from physical activity monitors in adults with multiple sclerosis. Adapt Phys Activ Q. 2007;24(3):245–253.
25. Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an Expanded Disability Status Scale (EDSS). Neurology. 1983;33(11):1444–1452.
26. Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol Res Pract. 2009;40(5):532–538.
27. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
28. Goldman MD, Motl RW, Scagnelli J, Pula JH, Sosnoff JJ, Cadavid D. Clinically meaningful performance benchmarks in MS. Neurology. 2013;81(21):1856–1863.
29. Guralnik JM, Ferrucci L, Pieper CF, et al Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the Short Physical Performance Battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–M231.
30. Bodling AM, Denney DR, Lynch SG. Cognitive aging in patients with multiple sclerosis: a cross-sectional analysis of speeded processing. Arch Clin Neuropsychol. 2009;24(8):761–777.
31. Healy GN, Matthews CE, Dunstan DW, Winkler E, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-2006. Eur Heart J. 2011;32(5):590–597.
32. Bakshi R. Fatigue associated with multiple sclerosis: diagnosis, impact and management. Mult Scler. 2003;9(3):219–227.

