Combined training improves walking mobility
Why is this important to me?
Walking problems tend to occur among individuals who have lived with MS for a long time. MS can affect several physiological systems that are used in walking, resulting in aerobic deconditioning (that is, being out of shape), muscle weakness, and balance problems. These changes in your physiology can sometimes make walking more difficult. Recent clinical trials examining ways to help stroke patients walk better showed that exercise including both cardiorespiratory and strength exercise improved various aspects of walking for these patients. Based on the success of using combined cardiorespiratory and strength exercise programs in stroke patients, the authors investigated whether an exercise program that addresses those physiological systems affected by MS can improve walking ability in people with MS.
What is the objective of this study?
Thirteen people with MS who had walking problems were enrolled in an exercise program designed to provide aerobic, resistance, and balance training. The authors compared walking ability before and after the 8-week program. After 8 weeks of the exercise program, the authors reported:
- 17% improvement in the Multiple Sclerosis Walking Scale-12 score, which is a self-reported measure of the impact of MS on walking.
- 16% improvement in the Timed 25-foot Walk, which measures walking speed.
- 19% improvement in the Timed Up & Go test, which measures walking initiation and mobility.
- Overall 7% improvement in functional walking, which includes gait speed, stride length, and other measures related to gait.
The results suggest that participating in a combined cardiorespiratory and strength exercise program can be effective in improving your walking ability. Interestingly, the programs were designed to fit wit the individual patient's personal preferences, a feature that can help to avoid the common pitfall of boredom in exercise regimens. The authors also considered each person's symptoms and motivation level in designing their exercise program. Finally, not all participants achieved the maximum exercise time of 60 minutes per session by week 8. Thus, with a wide variety of participation levels and exercises to choose from, people with MS can experience a benefit regarding their walking ability by performing exercises that improve multiple physiological systems.
Future studies should measure other aspects of walking ability (self-reported ability, performance, and gait measurements). Studies with a larger number of participants may help to .to design an exercise program for patients more precisely. Such studies should also address participants’ fatigue, a common symptom of MS, while participating in an exercise program.
How did the authors study this issue?
The authors enrolled 13 people with MS with significant walking disability (Expanded Disability Status Scale (EDSS), 4.0-6.0; 5 men and 8 women; mean age, 51.5 years; age range, 23-64 years; average time since MS diagnosis, 11.2 years). Seven participants could walk independently, and the other six used either a cane or a walker.
A moderately intense exercise program was designed by a physical therapist and included:
- aerobic exercises such as pedaling, treadmill walking, rowing, etc.
- resistance exercises such as squats and knee and ankle exercises with resistance bands
- balance exercises such as single-leg stands, heel-toe line walking, etc.
Participants performed the exercises 3 times a week for 8 weeks. Initially, each exercise type was performed for 5 minutes each (15 minutes per session), and the duration gradually increased to 20 minutes each (60 minutes per session). Participants were allowed to choose exercises they preferred, and therapists adjusted the exercises performed according to a participant’s muscle weakness and balance problems, if present.
Before the exercise program began and after 8 weeks of exercise, participants performed various tests to measure their self-reported walking ability, walking speed, walking initiation, and gait characteristics.
| SHARE: | |||||
Original Article
Combined Training Improves Walking Mobility in Persons With Significant Disability From Multiple Sclerosis: A Pilot Study
Journal of Neurologic Physical Therapy
Robert W. Motl, PhD, Douglas C. Smith, PhD, Jeannette Elliott, PT, Madeline Weikert, BS, Deirdre Dlugonski, BS, and Jacob J. Sosnoff, PhD
Background and Purpose: The disabling consequences of multiple sclerosis (MS) emphasize the significance of developing physiologically relevant strategies for rehabilitation of function. This pilot study examined changes in walking function associated with combined exercise training consisting of aerobic, resistance, and balance activities in persons with MS who had recent onset of gait impairment.
Methods: Thirteen participants with significant disability due to MS (Expanded Disability Status Scale range = 4.0-6.0) completed the Multiple Sclerosis Walking Scale–12, 2 trials of the Timed 25-Foot Walk, the Timed Up & Go, and functional ambulation profile score derived from 4 walking trials on an instrumented walkway (GaitRite) before and after an 8-week training period. The training program was designed by a physical therapist and was performed 3 days per week under the supervision of an exercise specialist. In week 1, the session was 15 minutes in duration (ie, 5 minutes of each mode of exercise), session durations were increased by approximately 5 minutes per week up to a maximum of 60 minutes in week 8 (ie, 20 minutes of each mode of exercise).
Results: There were significant improvements in Multiple Sclerosis Walking Scale–12 scores (Mpre = 56.0, Mpost = 46.7, P = 0.03, d = 0.56), Timed 25-Foot Walk (Mpre = 11.7, Mpost = 9.8, P = 0.004, d = 0.90) and Timed Up & Go (Mpre = 16.0, Mpost = 13.0, P = 0.01, d = 0.72) performance, and functional ambulation profile score (Mpre = 72.8, Mpost = 77.6, P = 0.02, d = 0.65).
Discussion and Conclusion: These results suggest that a moderately intense, comprehensive, combined exercise training program represents a rehabilitation strategy that is associated with improved walking mobility in a small sample of persons with MS who have recent onset of gait impairment.
Introduction
Some of the disabling consequences of multiple sclerosis (MS) include aerobic deconditioning, muscle weakness, and balance abnormalities, and such changes can impact walking mobility.1,2 Those consequences underscore the importance of developing physiologically relevant strategies for rehabilitation of function.3 There is evidence that physical exercise training can improve walking mobility in MS,4,5 but the existing literature has some deficiencies.6 One deficiency is that researchers have often included only a single mode of exercise training that does not account for the decline of multiple physiological systems (eg, aerobic deconditioning, muscle weakness, and balance dysfunction) that manifest in impaired walking mobility.6,7 In addition, prior studies of exercise in persons with MS have included only a limited set of outcome measures for quantifying walking mobility and have not focused on persons with MS who have significant disability as defined by benchmarks for cumulative mobility disability according to the Expanded Disability Status Scale (EDSS) scores.8
We based the development and testing of a combined exercise training program for persons with MS who have significant disability on previously randomized controlled trials in stroke. For example, a recent Cochrane review examined the effects of exercise training (ie, cardiorespiratory, strength, or both) on primary outcomes of death, dependence, and disability, along with secondary outcomes of physical fitness, mobility, and physical function, in patients with stroke.9 The review located 24 trials with 1147 participants with exercise regimens comprising cardiorespiratory (11 trials), resistance (4 trials), and mixed training (9 trials). The overall conclusions were that cardiorespiratory training that involved walking was associated with improved maximum walking speed, walking endurance, and reduced dependence during walking. The literature was characterized by too few resistance training and mixed training trials for conclusions about changes in mobility outcomes. Collectively, research in stroke largely paralleled the conclusions and recommendations for research in advanced stages of MS.
The present pilot study examined the changes in participant-rated, performance, and kinematic markers of walking mobility associated with an 8-week period of moderately intense combined exercise training (ie, equivalent amounts of aerobic, resistance, and balance training modalities) in participants with MS who had EDSS scores between 4.0 and 6.0. We hypothesized that subjects would self-report improvements in walking mobility, and these would be accompanied by positive changes in walking performance and spatiotemporal parameters of gait.
METHODS
Participants
We recruited persons with MS who had problems with walking mobility and who resided in central Illinois for participation in a supervised exercise training pilot study. This was accomplished through mail distribution of flyers among the 30 persons with MS in our database who had Patient Determined Disease Steps scale10 scores of 3, 4, or 5; the Patient Determined Disease Steps was used to as a screen to identify persons with EDSS scores that satisfied inclusion criteria. The inclusion criteria were physician-confirmed diagnosis of MS, EDSS score between 4.0 and 6.0, relapse free over the previous 6 months, age between 18 and 65 years, sedentary (ie, less than 3 days per week of exercise over previous 6 months), and physician approval for undertaking the exercise program
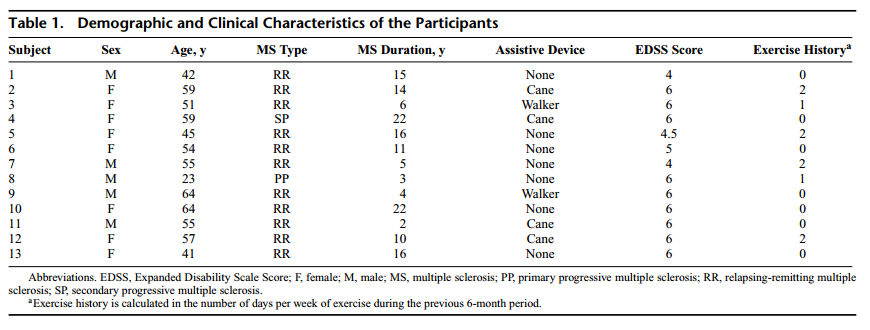
Seventeen of the 30 persons we identified in our database underwent screening, and 13 persons (5 men/8 women) with a diagnosis of MS (11 relapse-remitting MS; 1 secondary progressive MS; 1 primary progressive MS) and EDSS score of 4 to 6 (median = 6) volunteered to participate in the current pilot study. The 4 persons who underwent screening but did not participate expressed other time commitments as the basis for not volunteering. Participants ranged in age between 23 and 64 years with a mean of 51.5 years (SD = 11.3 years). The average time since diagnosis of MS was 11.2 years (SD = 6.9 years) with a range between 2 and 22 years. Of the 13 participants, 7 were independently ambulatory, 4 walked with single-point assistance, and 2 walked with 2-point assistance during daily life. Participants reported exercising a median of 0 (range = 0-2) days per week over prior 6 months.
All participants provided written informed consent to participate in the study, which had been approved by the University of Illinois at Urbana–Champaign institutional review board. We paid participants $50 for undertaking the testing ($25 for baseline and follow-up each), and payment was not linked with completion of the exercise training protocol. At the time of enrollment, all participants were using a diseasemodifying pharmacologic therapy (Avonex, n = 2; Betaseron, n = 3; Copaxone, n = 4; Rebif, n = 3; Tysabri, n = 1). The demographic and clinical characteristics for each of the 13 participants are provided in Table 1.
Outcome Measures
The outcome measures consisted of the Multiple Sclerosis Walking Scale–12 (MSWS-12) as a participant reported outcome of the impact of MS on walking,11 the T25FW as a performance measure of walking speed,12 the Timed Up & Go (TUG) as a performance measure of walking initiation and upright mobility13 and the functional ambulation profile (FAP) score of a commercially available instrumented walkway (GAITRite, CIR systems, Inc, Havertown, Pennsylvania). The FAP score is intended to represent a measure of gait efficiency and is based on the relationship among leg length, step length, and step time. The FAP score has been validated in persons with MS.14 In addition to the FAP score, the instrumented walkway provided measures of walking speed, cadence, stride length, step time, base of support, and percentages of gait cycle spent in double support, single support, and swing phase as spatial and temporal measures of gait.
Testing Procedures
Participants underwent an interview by the lead investigator (R.W.M.) for generating an EDSS score, completed self-report measures (demographics scale and MSWS-12), undertook 2 trials of 2 walking performance tests (T25FW and TUG), and then performed 4 trials of walking on the instrumented walkway. The order was always the same and participants received between 5 and 10 minutes of seated rest after each of the short walking tests. Those procedures were undertaken before and after the 8-week period of combined exercise training.
Exercise Training Protocol
The protocol was designed by an experienced physical therapist and involved a combined exercise-training program that was delivered by a trained exercise specialist 3 days per week over an 8-week period (ie, 24 sessions). The exercise program was generic, but participants did report affinities for particular exercises that were integrated into the program by the exercise specialist with the guidance of a physical therapist. The exercise specialist integrated exercise preferences, while accounting for existing muscle weaknesses and balance defi- ciencies; the deficiencies were identified on the basis of manual muscle testing for weakness assessments combined with professional judgment based on observation of the participants. The 8-week period of training was selected on the basis of feasibility for a pilot study and consistency in duration with effective interventions in previous research of exercise training and walking mobility in MS.3
All sessions began with 5 minutes of warm-up using a hand-crank cycle ergometer and ended with 10 minutes of lower extremity stretching. The latter involved common lower extremity muscle stretches plus stretches for the specific needs of the participants based on the exercise specialist’s professional judgment. Each training session was divided into aerobic exercise (ie, leg cycle ergometry, treadmill walking, elliptical, or seated rowing exercise), resistance exercise (ie, squats, knee flexion/extension, and ankle dorsiflexion/plantar flexion using resistance bands), and balance activities (ie, single-leg stands, figure eights, stair stepping, and heel-to-toe line walk), in nearly equal proportions. Participants were encouraged to participate in all types of aerobic exercise; we did not presume that all aerobic activities would be equivalent, but rather intended to provide variety on the basis of individual preferences and avoiding boredom.
The duration of each mode of exercise was gradually increased from 5 minutes in week 1 (ie, 15 minutes of total exercise) up to 20 minutes in week 8 (ie, 60 minutes of total exercise). The exercise was intended to be moderately intense, and a Borg’s scale of rating of perceived exertion (RPE)15 was targeted for level 13 (ie, “somewhat hard” exercise) by all participants over the 8-week period for all 3 types of exercise. The RPE data were collected immediately after the training sessions and did not vary considerably over time, likely because we provided standardized instructions and training to maintain the target intensity on the basis of this perceptual scale. Whereas the intent was that the duration of each of the 3 modes of exercise would be equivalent, not all participants achieved 20 minutes of each exercise by the end of the program; we felt that the flexibility in the program was necessary to accommodate for variation in MS symptoms and motivation. The training took place under the direct supervision of the exercise specialist with support of research assistants in an accessible gymnasium. The research assistants also recorded daily attendance and RPE for monitoring adherence to the exercise training protocol.
Statistical Analysis
Descriptive and inferential analyses were performed in SPSS Statistics, Version 19.0 (IBM, Chicago, Illinois). Values are presented as mean score ± standard deviation (SD) unless otherwise noted (eg, median score for EDSS). The inferential analysis involved paired-samples t tests comparing walking mobility measures obtained before (pretrial) and after (posttrial) the 8-week period of training. Significance was accepted as α ≤ 0.05 for a 1-tailed test, given our directional hypothesis. We did not correct for multiple tests, given the pilot nature of the study. We further did not conduct analysis of covariance controlling for variables such as age, medications, and compliance, given the small sample size and subsequent reduction in degrees of freedom per covariate. The magnitude of change in each walking mobility outcome was based on the Cohen d (difference in the mean scores divided by the SD of the change in the mean scores over time). Using the SD of change in the mean scores over time in computing the Cohen d has been suggested by Rosenthal16 because it accounts for the correlation between the repeated measures over time; this would not be accomplished with the pooled SD. Guidelines of 0.2, 0.5, and 0.8 were adopted for interpreting the effect size as small, moderate, or large, respectively.17 We further expressed change as a percent of change from baseline value (ie, [pretrial value − posttrial value] / pretrial value × 100).
RESULTS
Exercise Adherence and Compliance
The participants attended an average of 19.4 (SD = 4.8; range = 10-24) sessions. This equated with an adherence rate of 81% over the 8-week period. The average RPE over the 8-week period was 13.1 (SD = 1.3; range = 11.6- 16.2), which corresponds with a perceived exertion level of “somewhat hard” over the 8-week period and indicates that the training was at least moderately intense.
Walking Mobility Outcomes
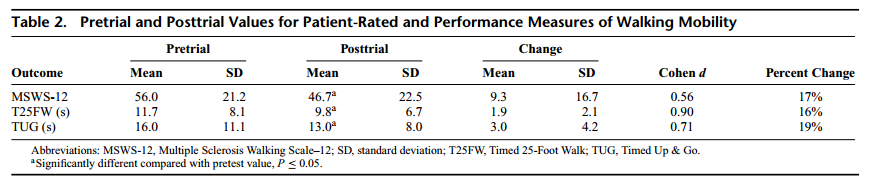
The descriptive statistics for the MSWS-12, T25FW, and TUG are provided in Table 2, and the pretest values are consistent with samples of persons with MS who have EDSS scores of 4.0 to 6.0 and significant walking impairments.11,12,18 There were significant improvements in MSWS-12 (t = 2.02, P = 0.03), T25FW (t = 3.26, P = 0.004), and TUG (t = 2.59, P = 0.01) scores. The effect sizes of 0.56, 0.90, and 0.71 were moderate to large for the changes in MSWS-12, T25FW, and TUG, respectively, with corresponding percent improvements of 17%, 16%, and 19% relative to baseline scores for the 3 measures. These effect sizes are larger than previously reported in a meta-analysis of exercise training and walking mobility in persons with MS.5 Importantly, removing the 2 cases of progressive MS and then running the analyses did not affect the results of the paired-samples t tests.
Spatiotemporal Parameters of Gait
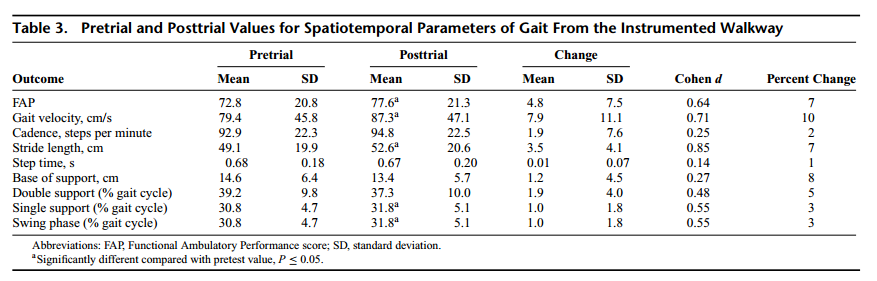
Descriptive statistics for the spatiotemporal parameters are provided in Table 3. The pretest value for the FAP is significantly lower than the mean value reported in previous research on persons with MS1,14 and is outside the range for normal gait (ie, 85-100). There was a significant improvement in the overall FAP score (t=2.33, P=0.02). Change in the FAP score had a moderate effect size of 0.64 with a corresponding percent improvement from baseline of 7%. The change in overall FAP score coincided with improvements in gait velocity (t = 2.57, P = 0.01), stride length (t = 3.09, P = 0.005), single support (t = 1.95, P = 0.03), and swing phase (t = 1.94, P = 0.04); the change in double support time showed a trend toward improvement (t = 1.66, P = 0.06). Change in gait velocity, stride length, single support, swing phase, and double support had moderate to large associated effect sizes of 0.71, 0.85, 0.55, 0.55, and 0.48, respectively, with percent improvements from baseline scores of 10%, 7%, 3%, 3%, and 5%; the other parameters from the instrumented walkway were unchanged in this pilot study.
DISCUSSION
The primary novel finding from the present pilot study was that an 8-week period of an exercise program containing aerobic, resistance, and balance training was associated with improvements in participant-rated, performance, and kinematic markers of walking mobility in a small sample of persons with MS who had significant disability (ie, EDSS scores between 4.0 and 6.0, and lower than previously reported mean FAP scores for this population). The participants self-reported an improvement in walking mobility on the MSWS-12. This was accompanied by positive changes in walking performance on the T25FW and TUG and improvements in spatiotemporal parameters of gait. The effect sizes for improvements in the MSWS-12, T25FW, TUG, and spatiotemporal parameters were generally moderate to large in magnitude and exceeded the average effect reported in a meta-analysis of exercise training and walking mobility in MS.5 Collectively, the results of this pilot study support the benefits of a relatively brief, moderately intense, combined exercise training intervention for improving walking mobility in a small sample of persons with MS who have reached a benchmark of gait impairment.
This pilot study builds upon limitations of previous research that has been summarized in a meta-analysis on exercise training and walking mobility among persons with MS.5 That meta-analysis identified 43 published exercise training studies published between 1960 and 2007, with 22 studies having sufficient data to compute effect sizes (Cohen d). Sixty-six effect sizes were retrieved from the 22 publications with 609 MS participants and yielded an overall weighted mean effect size of g = 0.19 (95% CI = 0.09, 0.28); g is an effect size that is weighted by sample size in meta-analysis and is comparable with Cohen d. The cumulative evidence supported that exercise training was associated with a small improvement in walking mobility among persons with MS; however, the vast majority of studies were conducted using samples with minimal mobility disability (ie, EDSS scores of ≤ 4.5) and only 1 mode of exercise (ie, aerobic or resistance training). The present study included both persons with MS who had onset of mobility impairment (ie, EDSS scores of 4.0-6.0) and 3 modes of exercise (ie, combination of aerobic, resistance, and balance training), and the average effect size across the 4 main outcome measures (ie, MSWS-12, T25FW, TUG, and FAP) was d = 0.71. This supports the value of developing and testing a comprehensive exercise training program that targets declines of multiple physiological systems (eg, aerobic deconditioning, muscle weakness, and balance dysfunction) as an approach for improving walking mobility in a large sample of persons with MS with onset of gait impairment.
We note that the improvements in walking mobility were seemingly based on beneficial changes in spatiotemporal parameters of the gait cycle. Collectively, this multidimensional assessment provides a comprehensive view of the improvements in walking mobility in association with the combined exercise training intervention. The observation of change in participant-rated, performance, and kinematic outcomes provides consistent evidence for the improvement in walking mobility that was observed in the present study of combined exercise training. This same multidimensional assessment might be useful in subsequent research on the rehabilitation of mobility in MS.
The strengths of this pilot study are the inclusion of a combined exercise-training stimulus and comprehensive set of outcome measures as well as a defined sample with onset of mobility impairment. Whereas similar pilot studies of exercise training in MS have been performed, these prior studies have focused on either resistance training or aerobic training.19–21 Whereas our sample was small, it was adequately powered to detect moderate and larger effects using a statistical analysis that accounted for repeated measurements over time. The short training period was selected for this pilot study on the basis of recommendations of a previous meta-analysis,5 and likely optimized compliance with the prescription for short-term improvements in walking mobility, but would not be appropriate for long-term maintenance of function over time. We did not measure fatigue as we were focusing on capturing improvements in walking mobility as a significant outcome in persons with MS who have EDSS scores between 4 and 6. This does not imply that fatigue is unimportant, but rather our focus on maintaining a moderately intense level of activity based on RPE. Accordingly, we believe that future research should capitalize on the positive findings of this pilot study for better designing and testing the effectiveness of combined exercise training for improving walking mobility, physiological function, fatigue, or other symptoms using a larger, randomized controlled trial in persons with MS. Such a study will signifi- cantly advance our understanding of designing physiologically relevant strategies for rehabilitation of function in MS.3 This is critical given the limited efficacy of disease-modifying therapies for stopping the accumulation of walking problems in the advanced stages of MS.8
Limitations
This study had a number of limitations including lack of a control or comparison condition, small sample size, short intervention period, and no follow-up assessment. Whereas a control condition would be appropriate for a true clinical trial, we believed that a pilot study such as that described herein is a necessary step for designing a randomized, controlled clinical trials. The small sample did not permit an examination of other variables such as actual EDSS score, MS duration or clinical course, exercise mode, sex, age, or symptoms as moderators or confounders of the improvements in walking mobility associated with combined exercise training. Furthermore, the small sample size did not permit analysis of covariance to control for variables such as age, medications, and compliance, given the subsequent reduction in degrees of freedom per covariate. The small sample size may limit generalizability. The lack of a follow-up further did not allow for examination of maintenance of the improvements in walking mobility after cessation of the combined exercise training. We further measured neither physiological changes such as aerobic capacity, muscle strength and function, and postural control as mechanisms for the improvement in ambulatory outcomes nor the symptom of fatigue.
CONCLUSIONS
The results of this study indicate that persons with MS who have significant disability and recent onset of gait impairment can benefit from participation in a program of moderately intense exercise. A program of combined exercise training that incorporates aerobic, resistance, and balance activities appears to have beneficial influence on both participantperceived walking mobility and objective measures of walking performance.
REFERENCES
1. Kalron A, Achiron A, Dvir Z. Muscular and gait abnormalities in persons with early onset multiple sclerosis. J Neurol Phys Ther. 2011;35:164-169.
2. Motl RW, Goldman M. Physical inactivity, neurological disability, and cardiorespiratory fitness in multiple sclerosis. Acta Neurol Scand. 2011;123:98-104.
3. Kraft GH. Rehabilitation still the only way to improve function in multiple sclerosis. Lancet. 1999;354:2016-2017.
4. Reitberg MB, Brooks D, Uitdehaag BMJ, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2004;(3):CD003980.
5. Snook EM, Motl RW. Effect of exercise training on walking mobility in multiple sclerosis: a meta-analysis. Neurorehabil Neural Repair. 2009;23:108-116.
6. Motl RW, Goldman MD, Benedict RHB. Walking impairment in patients with multiple sclerosis: exercise training as a treatment option? Neuropsychiat Dis Treat. 2010;6:767-774.
7. Motl RW. Physical activity and irreversible disability in multiple sclerosis. Exerc Sport Sci Rev. 2010;38:186-191.
8. Confavreux C, Vukusic S. Natural history of multiple sclerosis. Brain. 2006;129:606-616.
9. Saunders DH, Greig CA, Mead GE, et al. Physical fitness training for stroke patients. Cochrane Database Syst Rev. 2009;(4):CD003316.
10. Hadjimichael O, Kerns RB, Rizzo MA, Cutter G, Vollmer T. Persistent pain and uncomfortable sensations in persons with multiple sclerosis. Pain. 2007;127:35-41.
11. Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ. Measuring the impact of MS on walking ability: The 12-item MS Walking Scale (MSWS-12). Neurology. 2003;60:31-36.
12. Kaufman M, Moyer D, Norton J. The significant change for the Timed 25-foot Walk in the Multiple Sclerosis Functional Composite. Mult Scler. 2000;6:286-290.
13. Nilsagard Y, Lundholm C, Gunnarsson LG, Dcnison E. Clinical relevance using timed walk tests and “Timed Up & Go” testing in persons with multiple sclerosis. Physiother Res Int. 2007;12:105-114.
14. Givon U, Zeilig G, Achiron A. Gait analysis in multiple sclerosis: characterization of temporal-spatial parameters using GAITRite functional ambulation system. Gait Posture. 2009;29:138-142.
15. Borg GAV. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377-381.
16. Rosenthal R. Meta-analytic Procedures for Social Research. Newbury Park, CA: Sage Publications; 1991.
17. Cohen J. Statistical Power Analysis for the Behavioral Sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
18. Motl RW, Snook EM. Confirmation and extension of the validity of the Multiple Sclerosis Walking Scale–12 (MSWS-12). J Neurol Sci. 2008;268:69-73.
19. Gutierrez GM, Chow JW, Tilman MD, McCoy SC, Castellano V, White LJ. Resistance training improves gait kinematics in persons with multiple sclerosis. Acrh Phys Med Rehabil. 2005;86:1824-1829.
20. Kileff J, Ashburn A. A pilot study of the effect of aerobic exercise on people with moderate disability multiple sclerosis.Clin Rehabil. 2005;19:165- 169.
21. Newman MA, Dawes H, van den Berg M, Wade DT, Burridge J, Izadi H. Can aerobic treadmill training reduce the effort of walking and fatigue in people with multiple sclerosis: a pilot study. Mult Scler. 2007;13:113-119.
