Multiple Sclerosis and Exercise
Why is this important to me?
If you have MS, physical exercise can increase your energy levels, improve your walking ability and physical function, and provide a higher quality of life. Some symptoms of MS can reduce one's ability to exercise and therefore, many people with MS are sedentary and less likely to participate in an exercise program. Because of the benefits of exercise, you should work with your health care professionals to establish the most realistic exercise goals based on your abilities.
What is the objective of this study?
Tolerance for performing exercise is lower in people with MS than in healthy people, and maximum exercise ability is lower with worse disability. Compared to healthy people, you may:
- Generate less power during exercise
- Have reduced aerobic ability
- Have reduced muscle strength
Possible MS-related reasons for these reduced exercise abilities include:
- Spasticity
- Reduced nerve conduction
- Reduced muscle metabolism
- Muscle weakness
- Sensory problems
- Certain MS medications
Although exercise does not affect MS progression, physical activity, which may involve aerobic exercise and/or resistance training, can improve your:
- Strength
- Endurance
- Aerobic fitness
- Fatigability
- Mobility
- Walking speed and capacity, and step performance
- Quality of life
Goals of your exercise program may include:
- Modifying your exercise program to reduce fatigue and risk of falling
- Addressing functional problems such as standing from a chair, foot dragging while walking, climbing stairs, and problems with activities of daily living
- Improving your strength, flexibility, range of motion, and balance
- Improving your cardiovascular function
- Remaining properly hydrated
You may be at increased risk of falling, and your symptoms and energy levels may vary. Thus, your exercise program should be carefully supervised, customized, and modified as needed. Other problems associated with MS such as heat sensitivity, spasticity, muscle weakness, sensory problems, and fatigue may affect your ability to perform upright exercise such as walking or running. Exercise programs should take this into consideration. If your symptoms are worsening, you should check with your healthcare provider and only continue to exercise with his or her approval.
Original Article
Multiple Sclerosis and Exercise
Strength and Conditioning Journal
Peter Ronai, MS, RCEP, CSCS*D, NSCA-CPT*D and Tom LaFontaine, PhD, RCEP, CSCS, NSCA-CPT
OVERVIEW OF MULTIPLE SCLEROSIS
Multiple sclerosis (MS) is a chronic neurologic disease affecting approximately 2.5 million and 400,000 individuals worldwide and within the United States, respectively (2). Most patients are commonly diagnosed between the ages of 20 and 40 (2,3,6). MS affects 2–3 times as many women as men (2). MS is characterized by random (affecting various sites in the body including the eyes, skeletal muscles, the bladder, etc) autoimmune attacks of and damage to the insulating myelin sheath (demyelinization) of the central nervous system and to motor (effector) axons (nerve fibers). Lesions in myelin can be present in the cerebral hemispheres, brainstem, and spinal cord. Loss of myelin negatively affects rapid smooth coordinated movement (2). Table 1 describes the common disease courses of MS and their prevalence. Persons with MS typically assume a more sedentary lifestyle than apparently healthy individuals (5).

There are a number of MS symptoms, which can negatively alter an individual’s ability to perform physical activities and to exercise. 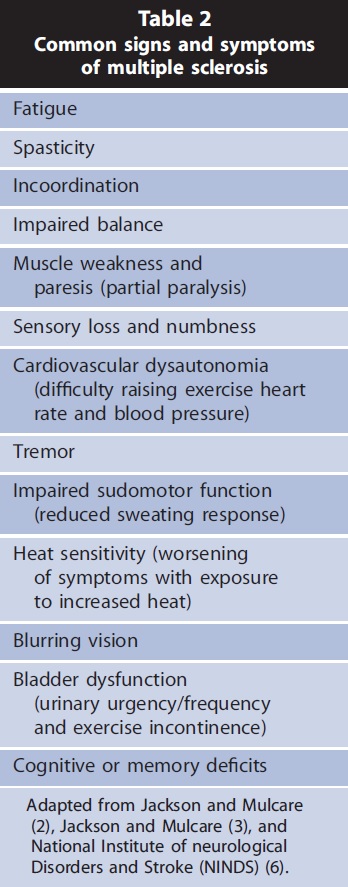 Table 2 describes common signs and symptoms of MS. MS is commonly diagnosed by patient history of attacks, magnetic resonance imaging of the brain and spinal cord, and analysis of spinal fluid during disease flare-ups for specific antibodies (2,6).
Table 2 describes common signs and symptoms of MS. MS is commonly diagnosed by patient history of attacks, magnetic resonance imaging of the brain and spinal cord, and analysis of spinal fluid during disease flare-ups for specific antibodies (2,6).
Life expectancy is linked to disability level. Most deaths are secondary to other non-MS–related complications like heart disease, hypertension, and diabetes (6). Disease-specific disability and severity are measured during a clinical examination with the Kurtzke expanded disability status scale (EDSS) (1,8).
To establish realistic physical activity goals, exercise professionals should know the ambulatory and functional status of their clients with MS before working with them. The EDSS is a 10-step scale with steps 1.0–4.5 referring to fully ambulatory status and steps 5.0–9.5 referring to increasing levels of ambulatory impairment.
EFFECTS OF MS ON THE EXERCISE RESPONSE
Exercise tolerance is reduced for people with MS, and maximal exercise capacity appears to be inversely related to EDSS level, with individuals who have a higher EDSS score possessing lower maximal and submaximal aerobic exercise (AE) capacities (2,4,12). Persons with MS have been observed to be more sedentary than apparently healthy age-matched individuals (5). Persons with MS generate 20–68% less power during leg cycling or combined leg-arm exercise testing protocols than healthy individuals (8). Maximal aerobic power (POmax) has been reported to be 31 and 24% lower on treadmill and bicycle ergometer testing, respectively, compared with healthy individuals (8). Nonspecific physical deconditioning is known to contribute to fatigue and general poor health in persons with MS (5). In addition, maximal muscle force measured during isokinetic testing has been shown to be consistently lower when matched to controls (2). Potential mechanisms for these observed deficiencies could include the following:
- Spasticity and/or cocontraction of opposing muscles
- Conduction block of demyelinated fibers
- Reduced muscle metabolic responses during voluntary exercise
- Muscle weakness because of fiber atrophy
- Sensory deficits (2)
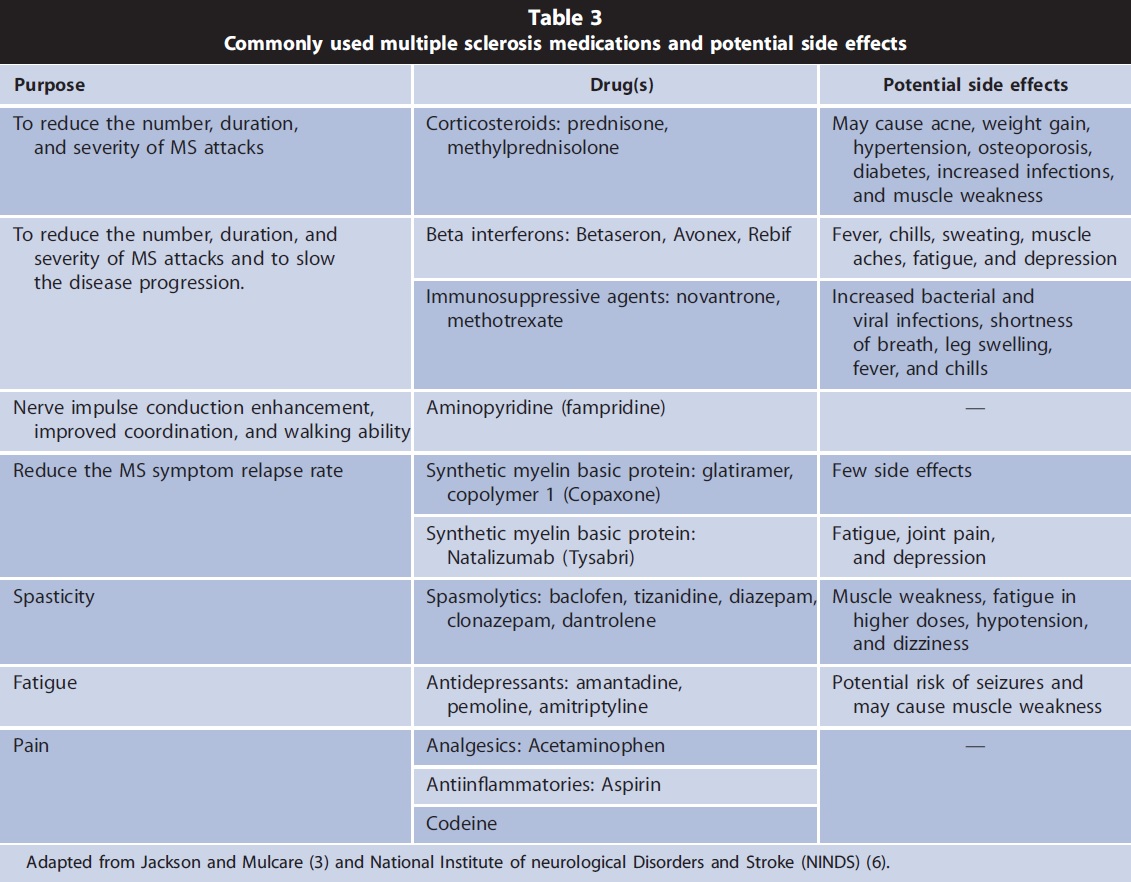
MEDICATIONS ASSOCIATED WITH MS
Several medications are used to modify and/or reduce the severity of the disease and number of exacerbations and to help manage symptoms of MS. Exercise response and tolerance can be altered by these medications (3). Table 3 describes commonly used medications and their potential side effects (3,6).
EXERCISE BENEFITS AND RISKS FOR PERSONS WITH MS
Previously, exercise was not often prescribed for persons with MS because it was believed to exacerbate symptoms and fatigue (1). Disease stage and severity determine individual responses to exercise. Although exercise training has no direct effects on prognosis or progression of MS, it may improve short-term and longterm physical fitness and functional performance (e.g., strength, endurance, aerobic fitness, fatigability, and mobility (3)). More recent studies indicate that moderate-intensity AEs improve physical fitness (1), mobility (4,11), walking speed (10) and capacity, exercise tolerance (9); reduce fatigue (5,7); and decrease disability (4,9). Improvements of 14.7, 18.2, and 27.7% in V_ O2peak, peak workload, and anaerobic threshold, respectively, have been observed in persons with MS participating in a supervised AE program (1).
Recent evidence suggests that resistance training (RT) is a safe effective form of exercise for persons with MS with mild to moderate disability (EDSS , 5) (5,10,12). Subjects engaged in an 8-week RT program consisting of 1 set of 10–15 repetitions at 70% of maximal voluntary contraction strength improved knee extension, plantarflexion, and stepping performance by 7.4, 52, and 8.7%, respectively (12). After participating in a 6-month, randomized, controlled exercise program consisting of 1 AE and 3 RT sessions per week, participants demonstrated significant improvements in walking speed, knee flexion strength, and upper extremity muscle endurance (10). In another study, participants engaging in a 3-month combined group and home RT program demonstrated significant improvements in exercise capacity, quality of life, and fatigue scores (5). Because some persons with MS are at an increased fall risk and their symptoms and energy levels can vary daily, AE and RT sessions should be supervised, individualized, and frequently modified. In addition, heat sensitivity, spasticity, sensory deficits, muscle weakness, and fatigue can preclude upright activities like walking and running and reduce tolerated exercise intensity and duration (2,3,6).
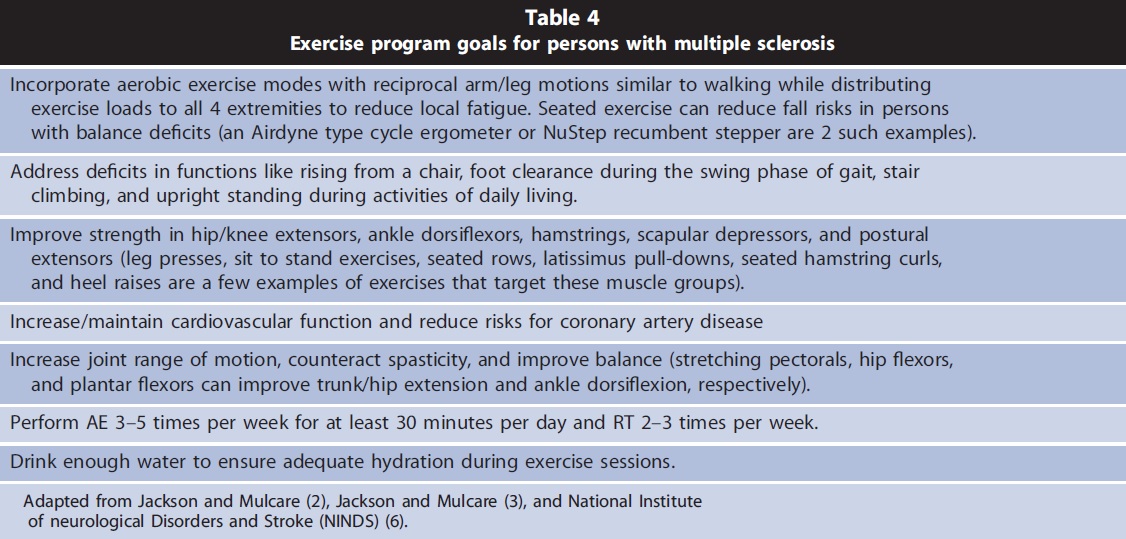
EXERCISE GOALS FOR PERSONS WITH MS
Exercise professionals should provide clients with MS close supervision and help reduce their fall risk both during exercise sessions and daily activities. They should monitor their clients for signs of fatigue and heat intolerance and encourage proper hydration. Exercise sessions should be modified as necessary to accommodate any fluctuations in client’s symptoms and energy level (2,3,6). Table 4 describes general exercise program goals for persons with MS.
Participants showing signs/symptoms of worsening disease or physical activity intolerance should be referred to their physician or health care provider. They should not resume their exercise program until their symptoms are under control and they have received medical clearance to do so.
SUMMARY
Exercise professionals can help persons with MS, who have been cleared by their physicians, engage in safe and effective exercise programs. Both AE and RT exercise programs can improve physical fitness, balance, mobility, performance of activities of daily living, and quality of life. The reader is directed to the ‘‘one on one’’ column for specific exercise programming guidelines, interventions, and strategies for persons with MS.
Peter Ronai is assuming a new role as an associate clinical professor in the Exercise Science Department at Sacred Heart University, Fairfield, CT.
Tom Lafonataine manages PREVENT Consulting Services and is an adjunct professor at the University of Missouri, Columbia, MO.
REFERENCES
1. Bjarnadottir O, Konradsdottir AD, Reynisdottir K, and Olafsson E. Multiple sclerosis and brief moderate exercise. A randomized study. Mult Scler 13: 776– 782, 2007.
2. Jackson K and Mulcare J. Multiple sclerosis. In: ACSM’s Resources for Clinical Exercise Physiology (2nd ed). Myers J and Nieman D, eds. Baltimore, MD: Lippincott Williams & Wilkins, 2009. pp. 34–43.
3. Jackson K and Mulchare J. Multiple sclerosis. In: ACSM’s Exercise Management for Persons with Chronic Diseases and Disabilities (3rd ed). Durstine JL, Moore GE, Painter PL, and Roberts SO, eds. Champaign, IL: Human Kinetics, 2009. pp. 321–326.
4. Kilef J and Ashburn A. A pilot study of the effect of aerobic exercise on people with moderate disability multiple sclerosis. Clin Rehabil 19: 165–169, 2005.
5. McCullagh R, Fitzgerald AP, Murphy RP, and Cooke G. Lon-term benefits of exercise on quality of life and fatigue in multiple sclerosis patients with mild disability: A pilot study. Clin Rehabil 22: 206–214, 2008.
6. National Institute of neurological Disorders and Stroke (NINDS). National Institutes of Health. Hope through research. http:// www.ninds.nih.gov/disorders/ multiple_sclerosis.htm?css=print. Updated December 1, 2008. Accessed: November 22, 2009.
7. Newman MA, Dawes H, van den Berg M, Wade DL, Burridge J, and Izadi H. Can aerobic treadmill training reduce the effort of walking and fatigue in people with multiple sclerosis? A pilot study. Mult Scler 13: 113–119, 2007.
8. Ponichtera-Mulcare JA, Mathews T, Glasser RM, Mathrews T, and Gupta SC. Maximal aerobic exercise of individuals with MS using three modes of ergometry. Clin Kinesiol 49: 4–13, 1995.
9. Rampello A, Franceschini M, Piepoli M, Antenucci R, Lenti G, Olivieri D, and Chetta A. Effects of aerobic training on walking capacity and maximal exercise tolerance in patients with multiple sclerosis: A randomized study. Phys Ther 5: 545– 555, 2007.
10. Romberg A, Virtanen A, Ruutiainen J, Aunola S, Karpi SL, Vaara M, Surakka J, Pohjolainen T, and Seppanen A. Effects of a 6-month exercise program on patients with multiple sclerosis: A randomized study. Neurology 63: 2034–2038, 2004.
11. Snook EM and Moti RW. Effects of exercise training on walking mobility in multiple sclerosis: A meta-analysis. Neurorehabil Neural Repair 23: 108–116, 2009.
12. White LC, McCoy SC, Castellano V, Gutierrez G, Stevens JE, Walter GA, and Vandenborne K. Resistance training improves strength and functional capacity in persons with multiple sclerosis. Mult Scler 10: 688–674, 2004.

