The Practice of Sport in Multiple Sclerosis
Original Article
The Practice of Sport in Multiple Sclerosis: Update
Current Sports Medicine Reports
Cecile Donze; Caroline Massot, MD; Patrick Hautecoeur; Helene Cattoir-Vue; and Marc-Alexandre Guyot
Abstract
The practice of sport by multiple sclerosis patients has long been controversial. Recent studies, however, show that both sport and physical activity are essential for these patients. Indeed, they help to cope with the effects of multiple sclerosis, such as fatigue, reduced endurance, loss of muscle mass, and reduction of muscle strength. The beneficial effects of physical activity on these patients have been underlined in several studies, whereas those of practicing sport have been the subject of fewer evaluations and assessments. The aim of this update is to report on the effects of sport on multiple sclerosis patients. The benefits of sport have been demonstrated in several studies. It helps multiple sclerosis patients to increase their balance, resistance to fatigue, mobility and quality of life. Several biases in these studies do not enable us to recommend the practice of some of these sports on a routine basis.
Introduction
Multiple sclerosis (MS) is a chronic autoimmune disease of the central nervous system. MS has an important impact on leisure activities like physical activity (PA) and social well-being. PA has long been controversial in MS with the fear of increasing fatigue and potentially causing relapses. The results of studies are now clearly stating that exercise practice does not worsen MS (14,15). On the contrary, several published analyses have found a beneficial effect of PA (30). Some studies in an animal model of MS (experimental autoimmune encephalomyelitis) were able to show the antiinflammatory effect of PA with a reduction of the development of clinical signs and even a possible delayed disease progression (31).
In several European countries, the term ‘‘sport’’ is used for all exercises and PA. However, we must draw a distinction between PA and sport. PA is defined by ‘‘any bodily movement produced by skeletal muscles that results in energy expenditure’’ (6). This includes the activities of daily living, such as sport, but also occupational activities, at work, or during leisure. Sport meanwhile is a PA that involves structured competitive situations, determined by rules. A variant of PA is adapted PA (APA) which is the science of evaluating physical capacity and intervention through PA among people with disabilities (42). The concept of APA is coming from Canada, and the term was introduced in Europe in 1973. The concept of ‘‘APA and Health’’ uses the positive effects of sport and PA on health by adapting the methods of practice, the context, and rules.
The first objective of PA in MS is to avoid the effects of a sedentary lifestyle. Indeed inactivity in the general population is a risk factor for cardiovascular disease, obesity, diabetes, and osteoporosis. Physical inactivity also is responsible for increasing fatigue, decreasing endurance, enhancing loss of muscle mass, and reducing muscle strength (11). In MS, symptoms including spasticity, muscle weakness, fatigue, imbalance, and deconditioning (10,13,46). An important point, when treating these patients, is to promote PA to fight against this deconditioning but also fatigue and other symptoms and eventually even improve disability and quality of life (QOL).
How People With MS Can Practice PA
The practice of PA quite often calls for rehabilitation programs or strengthening muscle programs. Rehabilitation programs include inpatient and outpatient rehabilitation programs. However, these programs also can be offered at home or in sports club, but patients need to be supervised by health professional (14,15). JM Charcot in his No 8 lesson already talked about management of these patients and had mentioned the importance of ‘‘rehabilitation through movement’’ (8). In 1953, Smith (47) published an article describing different exercises to perform at home adapted to the disability level. In 1984 Gehlsen et al. (22) proposed an aquatic exercise program for MS patientsto improve muscular strength, endurance, work, and power. The first randomized controlled trial was published in 1996, by Petajan et al. (39) who showed the feasibility and effectiveness of a PA program on QOL and endurance in these patients. The first guidelines for the practice of PA in MS were published in 1999 (40). Two types of exercises were then used alone or combined: resistance training program and strengthening muscle. Besides the codified rehabilitation programs, sport activities can be proposed.
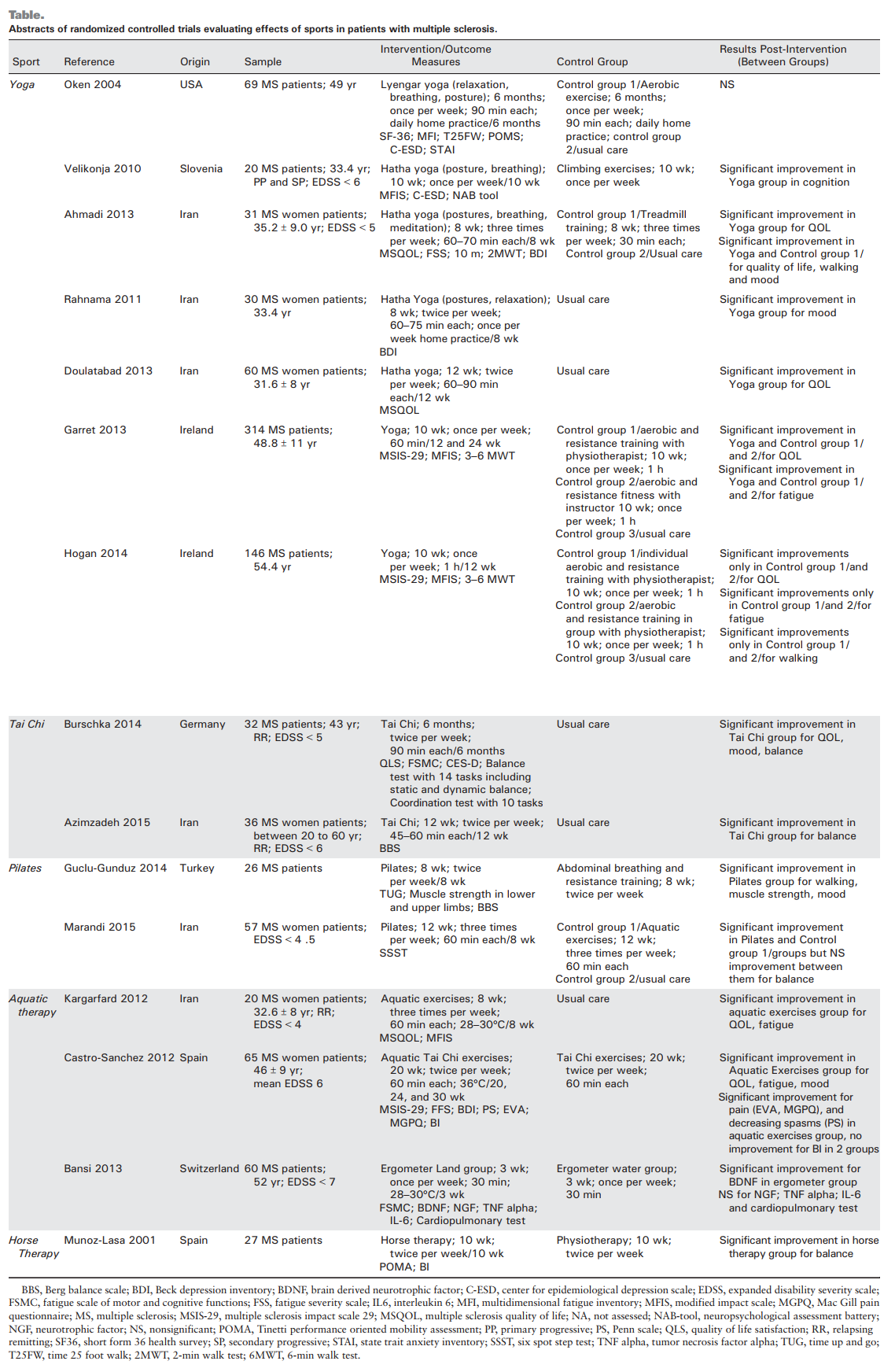
The aim of the article was to assess and report on studies evaluating the effects of sport on MS patients. All randomized controlled trials are summarized in the Table.
Yoga
Traditional yoga includes not only PA but also breathing and relaxation techniques and meditation. The ultimate goal is to unify mind, body, and spirit. The Cramer review and meta-analysis reported the beneficial effects of different types of yoga exercises (12). In a survey conducted in the United Kingdom, yoga sport is one of the most used complementary therapies in MS (17). Indeed, 31% of patients have practiced yoga in the year and 80% of them considered it as very effective. In the United States, a study of 2026 MS patients, reported 23% of patients practicing yoga regularly (51). The Cramer meta-analysis evaluated the efficacy of yoga in this pathology (12). Seven randomized controlled trials were selected with a total of 670 patients enrolled. All programs used physical exercises, breathing, and relaxation. Average program duration was 10 wk at a frequency of two to three sessions of 60 to 90 min-wk -1(1,16,21,25,38,41,49). Only one study examined the long-term effects (25). The results concluded improvement in fatigue and mood, no effect on QOL, strength, and cognitive functions. No severe adverse events were reported. There are many biases in these studies, and it seems difficult for now to recommend yoga in routine therapy even though it remains an interesting treatment option.
Tai Chi
Tai Chi Chuan or Tai Chi is an ancient Chinese martial art characterized by slow, controlled movements, combined with deep breathing and correct posture. The primary goal of Tai Chi is relaxation of the body and the mind. In MS, three pilot studies have shown an improvement in mood (36), QOL (26), balance (3,36), physical and mental health, and non-neuropathic pain (48). Two recent randomized controlled trials noted a positive effect of Tai Chi on balance and coordination compared to controls pursuing their usual activities (5,35). If these results are encouraging, biases persist, such as exclusively female populations for both studies, very different duration of interventions (2-6 months), small samples and a moderate level of disability, which makes it difficult to generalize the results to the entire MS population.
Pilates
Pilates was developed in the early twentieth century by Joseph Pilates. Its objectives are the development of deep muscles, improving posture, stabilizing muscles, and easing to maintain, improve or restore physical function. This mind-body exercise targets core balance muscles of the body by focusing on muscles responsible for posture and postural balance. It is based on six fundamental principles: concentration, control and balance of the spine, precision and fluidity responsible in harmonious movements, and breathing. This technique has been the subject of relatively little scientific publication, and few studies have been conducted on low back pain without results (50). In MS, four studies were conducted: a case series published in 2012 by Freeman showed a positive effect on walking, but further evidence is needed with studies with best methodological quality (19). Another pilot study evaluated the interest of Pilates used for 12 wk (twice per week) in a population of 15 MS patients in manual wheelchairs. The authors reported a significant improvement in sitting balance, a reduction of the impact of the disease in activity of daily living and pain in the upper limbs. Exercises were very well tolerated, and satisfaction was excellent (32). Two randomized controlled trials showed efficacy of Pilates on balance in MS population. Guclu-Gunduz compared Pilates method in 26 MS patients to a control group practicing exercises at home (23). The authors showed that Pilates method was more effective on balance, mobility, and strength. Marandi et al. (35) in 2013 compared three different programs (Pilates/ aquatic exercises/usual treatment) in 45 MS patients. The dynamic balance improved significantly in the aerobics and Pilates programs compared with the control group. These studies are promising but need to be confirmed by large-scale randomized controlled trials.
Aquatic Exercises
Aquatic exercises are particularly used in the context of resistance training and muscle strengthening. The benefits are numerous and are related to the relative ‘‘lightness’’ caused by the immersion of the body. Aquatic exercise benefits are muscular relaxation, a reduction in the risk of injury thank to the viscosity of water, a reduction of speed movement enabling proprioception improvement, and finally, a thermodynamic effect allowing a faster cooling of the body during PA (20). Aquatic environment, with the delayed thermoregulation in MS patients, was aimed at reducing the risk of body temperature escalation (20).
Gehlsen et al. (22) in 1984 showed an increase in strength, power and reduced fatigue after 10 wk of aquatic fitness program, made three times per week to 60% of maximum effort in water between 25-C and 27.5-C. Roehrs and Karst (43) showed positive effects on fatigue in patients with progressive MS after 12 wk of aquatic exercises (twice per week). Another study observed an improving balance and walking speed after 5 wk in the group with water aerobic exercises (44). Randomized controlled trials evaluating an aerobic program carried out for 8 wk compared two groups of MS patients (aerobic exercise vs standard therapy). The aerobic exercise group improved their QOL and reduced their fatigue (29). More recently, Marandi et al. (35) found that dynamic balance was improved after 12 wk of aquatic exercises performed three times per week. Finally, Bansi et al. (2) showed a significant increase in serum levels of brain derived neurotrophic factor in response to cardiopulmonary exercise after 3 wk of aquabiking. The authors conclude that aquabiking can activate regulatory pathways of the brain-derived neurotrophic factor which is involved in neuroplasticity (2,20). One randomized controlled study was conducted to relieve nociceptive pain of an MS population with a pool Tai Chi program (water at 36-C) compared with a control group doing the same Tai Chi program within water. After 20 wk, a significant effect on pain was obtained and maintained up to 30 wk (7). Aquatic environment exercises seem to be an effective way to improve fatigue, QOL, balance, strength, and nociceptive pain in this population.
Horse Therapy
Riding has been used for a long time as a therapeutic treatment. Chassaigne (9) in 1870 published his thesis in which he showed the benefit of this technique in different neurological pathologies on balance, joint flexibility, strength, and mood. Three noncontrolled trials have been conducted in MS. Mackay-Lyons in 1998 studied 10 patients who practiced 30 to 45 min of equitherapy twice a week for 9 wk. The results showed a subjective improvement on balance (33). Hammer, in a pilot study with 11 MS patients participating in a horse therapy program (30 minIwkj1 for 14 wk), showed balance improvement (24). Silkwood also found balance and walking improvement in a population of nine outpatients who completed the program 30 minIwkj1 for 14 wk (45). One randomized controlled trial was conducted by Munoz-Lasa in 2011 in which 27 outpatients were randomized into two groups (horse therapy vs physiotherapy). The authors noted significant improvement in balance and walking in the horse therapy group (37).
Other sports also have been evaluated in nonrandomized and uncontrolled pilot studies among which were kickboxing, climbing, and dancing. Two studies with a small sample of patients with low level of disability showed improvements on balance and walking through kickboxing activity (27,28). Rock climbing also has been tested in comparison to yoga and has shown an improved fatigue in 20 patients aged 25 to 50 yr with an Expanded Disability Status Scale score less than 6.5 (49). Finally, Salsa was proposed to eight MS patients with ambulation capacity at a rate of four times 60 minIwkj1 (34). Efficiency was found on balance, walking, and selfefficacy. Although the available literature on sport activity in MS is still quite poor, it remains promising in terms of efficiency on certain symptoms.
Nevertheless, there is a wide variety of functional and cognitive capacity in MS patients which may affect their ability for some modalities of exercise. Urinary control is a common symptom in MS patients. Patients may limit their hydration to help control urinary issues and would therefore need instruction to increase their hydration with increased activity levels. Fatigue, is another common symptom in MS (18). Because the interventions noted in this article revolve around resistance training and muscle strengthening, patients should be educated on the difference between systematic fatigue and momentary fatigue experienced with muscular strength and endurance training.
This also makes intensity of exercise hard to gauge, especially because autonomic controls will vary depending on the progression of the disease. However, rating of perceived exertion scale is a suitable method of gauging intensity and should be substituted (4).
In practice, most sports are possible and none are forbidden. They should just be adapted to the patient’s disability and personalized support should be provided, ideally by professional trainers.
Conclusion
PA is one type of care in patients with MS. Many beneficial effects have been shown in studies including balance, fatigue, mobility, and QOL. It allows for an action especially on the part of deconditioning and muscle weakness of peripheral origin but also may have an effect on disease progression. The effect on QOL and mood should not be neglected as well as the effects on health in general.
PA should be proposed to patients with MS so as to help them improve their different symptoms. Studies demonstrated many positive effects of PA especially on balance, fatigue, mobility, and QOL.
Deconditioning and muscle weakness of peripheral origin may be particularly improved by PA which also may have a positive effect on disease progression.
The authors thank Mrs. Dupont for proofreading and translating of the text.
The authors declare no conflict of interest and do not have any financial disclosures.
REFERENCES
1. Ahmadi A, Arastoo AA, Nikbakht M, et al. Comparison of the effect of 8 weeks aerobic and yoga training on ambulatory function, fatigue and mood status in MS patients. Iran Red Crescent Med J. 2013; 15:449Y54.
2. Bansi J, Bloch W, Gamper U, Kesselring J. Training in MS: influence of two different endurance training protocols (aquatic versus overland) on cytokine and neurotrophin concentrations during three week randomized controlled trial. Mult. Scler. 2013; 19:613Y21.
3. Binns EE, Taylor D. Does tai chi improve strength and balance in people with multiple sclerosisVthe current literature. Nz J Physiother. 2008; 36:83.
4. Borg GA. Scaling pain and related subjective somatic symptoms. 1998; 63Y7.
5. Burschka JM, Keune PM, Oy UH, et al. Mindfulness-based interventions in multiple sclerosis: beneficial effects of Tai Chi on balance, coordination, fatigue and depression. BMC Neurol. 2014; 14:165.
6. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985; 100(2):126Y31.
7. Castro-Sa´nchez AM, Matara´n-Pen˜ arrocha GA, Lara-Palomo I, et al. Hydrotherapy for the treatment of pain in people with multiple sclerosis: a randomized controlled trial. Evid. Based Complement Alternat. Med. 2012;2012:473963. [cited 2016 Jan 25] Available from: http://www.ncbi. nlm.nih.gov/pmc/articles/PMC3138085/.
8. Charcot JM. Lec¸on n-8. In: Lec¸ons sur les maladies du syste`me nerveux faites a` la salpeˆtrie`re. Paris: 1975.
9. Chassaigne DR. Physiologie de l’e´quitation de bon application a` l’hygie`ne et a` la the´rapeutique. (Cand. R. Chassaigne). [Internet]. 1870; [cited 2016 Feb 6] Available from: http://scholar.google.com/scholar?cluster=2519619498385721172& hl=en&oi=scholarr. 10. Chetta A, Rampello A, Marangio E, et al. Cardiorespiratory response to walk in multiple sclerosis patients. Respir. Med. 2004; 98:522Y9.
11. Convertino VA, Bloomfield SA, Greenleaf JE. An overview of the issues: physiological effects of bed rest and restricted physical activity. Med. Sci. Sports Exerc. 1997; 29:187Y90.
12. Cramer H, Lauche R, Azizi H, et al. Yoga for multiple sclerosis: a systematic review and meta-analysis. PLoS. One. 2014; 9. [cited 2016 Jan 24] Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4229199/.
13. Dalgas U, Stenager E, Ingemann-Hansen T. Multiple sclerosis and physical exercise: recommendations for the application of resistance-, endurance- and combined training. Mult. Scler. 2008; 14:35Y53. 14. Donze´ C. Neurorehabilitation in multiple sclerosis: an overview. Rev. Neurol. (Paris). 2007; 163:711Y9.
15. Donze´ C. Update on rehabilitation in multiple sclerosis. Presse Med. 2015; 44(4 Pt 2):e169Y76.
16. Doulatabad SN, Nooreyan K, Doulatabad AN, Noubandegani ZM. The effects of Pranayama, Hatha and Raja yoga on physical pain and the quality of life of women with multiple sclerosis. Afr. J. Tradit. Complement. Altern. Med. 2012; 10:49Y52.
17. Esmonde L, Long AF. Complementary therapy use by persons with multiple sclerosis: benefits and research priorities. Complement. Ther. Clin. Pract. 2008; 14:176Y84.
18. Ferguson B. ACSM’s guidelines for exercise testing and prescription, 9th Ed. 2014. J. Can. Chiropr. Assoc. 2014; 58:328.
19. Freeman JA, Gear M, Pauli A, et al. The effect of core stability training on balance and mobility in ambulant individuals with multiple sclerosis: a multi-centre series of single case studies. Mult. Scler. 2010; 16:1377Y84.
20. Frohman AN, Okuda DT, Beh S, et al. Aquatic training in MS: neurotherapeutic impact upon quality of life. Ann. Clin. Transl. Neurol. 2015; 2:864Y72.
21. Garrett M, Hogan N, Larkin A, et al. Exercise in the community for people with minimal gait impairment due to MS: an assessor-blind randomized controlled trial. Mult. Scler. 2013; 19:782Y9.
22. Gehlsen GM, Grigsby SA, Winant DM. Effects of an aquatic fitness program on the muscular strength and endurance of patients with multiple sclerosis. Phys. Ther. 1984; 64:653Y7.
23. Guclu-Gunduz A, Citaker S, Irkec C, et al. The effects of pilates on balance, mobility and strength in patients with multiple sclerosis. NeuroRehabilitation. 2014; 34:337Y42.
24. Hammer A, Nilsaga˚rd Y, Forsberg A, et al. Evaluation of therapeutic riding (Sweden)/hippotherapy (United States). A single-subject experimental design study replicated in eleven patients with multiple sclerosis. Physiother. Theory Pract. 2005; 21:51Y77.
25. Hogan N, Kehoe M, Larkin A, Coote S. The effect of community exercise interventions for people with MS who use bilateral support for gait. Mult. Scler. Int. 2014; 2014:109142.
26. Husted C, Pham L, Hekking A, Niederman R. Improving quality of life for people with chronic conditions: the example of t’ai chi and multiple sclerosis. Altern. Ther. Health Med. 1999; 5:70Y4.
27. Jackson K, Edginton-Bigelow K, Bowsheir C, et al. Feasibility and effects of a group kickboxing program for individuals with multiple sclerosis: a pilot report. J. Bodyw. Mov. Ther. 2012; 16:7Y13.
28. Jackson K, Edginton-Bigelow K, Cooper C, Merriman H. A group kickboxing program for balance, mobility, and quality of life in individuals with multiple sclerosis: a pilot study. J. Neurol. Phys. Ther. 2012; 36:131Y7.
29. Kargarfard M, Etemadifar M, Baker P, et al. Effect of aquatic exercise training on fatigue and health-related quality of life in patients with multiple sclerosis. Arch. Phys. Med. Rehabil. 2012; 93:1701Y8.
30. Latimer-Cheung AE, Pilutti LA, Hicks AL, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch. Phys. Med. Rehabil. 2013; 94:1800Y1828.e3.
31. Le Page C, Bourdoulous S, Be´raud E, et al. Effect of physical exercise on adoptive experimental auto-immune encephalomyelitis in rats. Eur. J. Appl. Physiol. Occup. Physiol. 1996; 73:130Y5.
32. van der Linden ML, Bulley C, Geneen LJ, et al. Pilates for people with multiple sclerosis who use a wheelchair: feasibility, efficacy and participant experiences. Disabil. Rehabil. 2014; 36:932Y9.
33. MacKay-Lyons M, Conway C, Roberts W. Effects of therapeutic riding on patients with multiple sclerosis: a preliminary trial. Physiother. Can. 1988; 40:104Y9.
34. Mandelbaum R, Triche EW, Fasoli SE, Lo AC. A pilot study: examining the effects and tolerability of structured dance intervention for individuals with multiple sclerosis. Disabil. Rehabil. 2016; 38:218Y22.
35. Marandi SM, Nejad VS, Shanazari Z, Zolaktaf V. A comparison of 12 weeks of pilates and aquatic training on the dynamic balance of women with mulitple sclerosis. Int. J. Prev. Med. 2013; 4(Suppl 1):S110Y7.
36. Mills N, Allen J, Carey-Morgan S. Does Tai Chi/Qi Gong help patients with multiple sclerosis? J. Bodyw. Mov. Ther. 2000; 4:39Y48.
37. Mun˜ oz-Lasa S, Ferriero G, Valero R, et al. Effect of therapeutic horseback riding on balance and gait of people with multiple sclerosis. G. Ital. Med. Lav. Ergon. 2011; 33:462Y7.
38. Oken BS, Kishiyama S, Zajdel D, et al. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004; 62:2058Y64.
39. Petajan JH, Gappmaier E, White AT, et al. Impact of aerobic training on fitness and quality of life in multiple sclerosis. Ann. Neurol. 1996; 39:432Y41.
40. Petajan JH, White AT. Recommendations for physical activity in patients with multiple sclerosis. Sports Med. Auckl. NZ. 1999; 27:179Y91.
41. Rahnama N, Namazizadeh M, Etemadifar M, et al. Effects of yoga on depression in women with multiple sclerosis. Journal of Isfahan Medical School. 2011; 29:483Y90.
42. Reid G, Stanish H. Professional and disciplinary status of adapted physical activity. Adapt Phys Act Q. 2003; 203:213Y29.
43. Roehrs TG, Karst GM. Effects of an aquatics exercise program on quality of life measures for individuals with progressive multiple sclerosis. J. Neurol. Phys. Ther. 2004; 28:63Y71.
44. Salem Y, Scott AH, Karpatkin H, et al. Community-based group aquatic programme for individuals with multiple sclerosis: a pilot study. Disabil. Rehabil. 2011; 33:720Y8.
45. Silkwood-Sherer D, Warmbier H. Effects of hippotherapy on postural stability, in persons with multiple sclerosis: a pilot study. J. Neurol. Phys. Ther. JNPT. 2007; 31:77Y84.
46. Slawta JN, Wilcox AR, McCubbin JA, et al. Health behaviors, body composition, and coronary heart disease risk in women with multiple sclerosis. Arch. Phys. Med. Rehabil. 2003; 84:1823Y30.
47. Smith EA. Home exercise devices. Phys. Ther. Rev. 1953; 33:21Y4.
48. Tavee J, Rensel M, Planchon SM, et al. Effects of meditation on pain and quality of life in multiple sclerosis and peripheral neuropathy: a pilot study. Int. J. MS. Care. 2011; 13:163Y8.
49. Velikonja O, )uri( K, Oºura A, Jazbec Sw. Influence of sports climbing and yoga on spasticity, cognitive function, mood and fatigue in patients with multiple sclerosis. Clin. Neurol. Neurosurg. 2010; 112:597Y601.
50. Wells C, Kolt GS, Marshall P, et al. Effectiveness of Pilates exercise in treating people with chronic low back pain: a systematic review of systematic reviews. BMC Med. Res. Methodol. 2013; 13:7.
51. Yadav V, Narayanaswami P. Complementary and alternative medical therapies in multiple sclerosisVthe American Academy of Neurology Guidelines: a commentary. Clin. Ther. 2014; 36:1972Y8.

