Perspectives on Physical Activity Among People with Multiple Sclerosis Who Are Wheelchair Users
Why is this important to me?
According to this article, people with MS may be less physically active than people without the disease, and people with advanced MS who use wheelchairs are even less physically active. Physical activity is important for improving the symptoms associated with your MS and is an important part of your self-care. Thus, understanding the daily factors that permit and prevent physical activity in people with MS who are wheelchair users is important for encouraging such behavior.
What is the objective of this study?
15 people with MS who used wheelchairs were analyzed and two main themes that emerged: 1. everyday experiences related to opportunities to be physically active and 2. physical activity experiences.
Everyday experiences
This theme explored social experiences and adaptations related to opportunities to be active.
The following parameters were related to the participant’s ability to physically participate in everyday activities:
- The use of devices that assist with mobility such as wheelchairs, walkers, and canes.
- Modifications of their home such as handrails and wheelchair-accessible showers.
- Adaptations to their car such as hand controls.
- A caregiver who assists the person with MS so he or she can participate in social activities.
Many of the above strategies may allow you to maintain your independence and to participate in family and social activities. However, overuse of these adaptations could also lead to dependency. As reported by the participants in this study, if you rely too much on a motorized wheelchair or an overprotective caregiver that does too much for you, you could lose your motivation to be active, become dependent on others, and get frustrated.
Physical activity experiences
This theme explored the perceived benefits of physical activity, the factors that prevent or allow people with MS who use wheelchairs to participate in physical activity and exercise, and the knowledge and guidance provided by health-care professionals about physical activity.
Participants reported that the benefits of physical activity were:
- Independence
- Improvement in strength, mobility, and symptoms such as fatigue
- Increased function and reduced tendency to fall
- Increased social participation
- Improved mood
Participants reported several factors that allowed them to participate in physical activity and that sometimes prevented participation when they were not available:
- Adaptive strategies such as being physically active at the right temperature
- Facilities with exercise equipment that was wheelchair accessible
- Positive social and behavioral factors such as positive feedback from others, goal setting, and following an enjoyable program
Health care providers provided guidance to increase physical activity. However, sometimes providers were not well informed and provided only minimally helpful advice.
Overall, maintaining physical activity if you have MS and use a wheelchair is likely to increase your quality of life. Low participation in physical activity may result when too many barriers and too few adaptations are available. Important steps toward increasing physical activity include an accessible environment and improved education of health care providers about promoting physical activity in people with MS who use wheelchairs.
How did the authors study this issue?
The authors interviewed 15 people (12 women; average age, 52 years) residing in the Midwestern US with advanced MS who used wheelchairs to understand themes that prevented them from participating in physical activity and what adaptations allowed them to be more active and independent. The participants were asked about their social participation, everyday experiences, lifestyle behavior, and physical activity and exercise.
Original Article
Perspectives on Physical Activity Among People with Multiple Sclerosis Who Are Wheelchair Users
Informing the Design of Future Interventions
International Journal of MS Care
Yvonne C. Learmonth, PhD; Ian M. Rice, PhD; Teresa Ostler, PhD; Laura A. Rice, PhD; Robert W. Motl, PhD
Background: People with advanced multiple sclerosis (MS) are less physically active than those with milder forms of the disease, and wheelchair use has a negative association with physical activity participation. Thus, wheelchair users with MS are doubly disadvantaged for accruing the benefits of physical activity and exercise. Appropriate physical activity and exercise interventions are needed for this population.
Methods: We undertook a qualitative study to explore the meanings, motivations, and outcomes of physical activity in wheelchair users with MS. We sought to understand daily opportunities to accumulate physical activity and exercise, and to identify perceived barriers, facilitators, and benefits that might inform the design of future interventions.
Results: We interviewed 15 wheelchair users (mean age, 52 ± 8.8 years; n = 12 women). Data were transcribed and analyzed to identify and explore common themes. Our first theme was the reduced opportunity to participate in physical activity due to participants’ dependence on mobility devices, environmental adaptations, and tangible support. Our second theme was the importance of incorporating physical activity and exercise into the everyday environment, highlighting the need for adaptive exercise and accessible environments. This indicated the need to incorporate behavior change modulators into physical activity and exercise interventions for those with advanced MS. Health-care professionals played an important role in promoting increased physical activity and exercise participation in those with advanced MS.
Conclusions: Our findings may inform future interventions to increase initiation and maintenance of physical activity and exercise among people with advanced MS. Int J MS Care. 2015;17:109–119.
Multiple Sclerosis (MS) is a chronic, nontraumatic disease of the central nervous system (CNS) with a prevalence exceeding 2 million people globally.1 Depending on its location, the CNS damage can result in loss of mobility, symptoms of depression and fatigue, reduced quality of life (QOL), and decreased community participation over time.2 One behavioral strategy for improving the symptoms associated with MS involves initiating and maintaining physical activity and exercise.3,4 Moreover, exercise and physical activity have been identified by a consensus panel of experts as critical components of comprehensive MS care4 and are acknowledged as significant components of patient self-management.5 Physical activity is defined as any bodily movement produced by contraction of skeletal muscles resulting in energy expenditure, whereas exercise—one type of physical activity—is defined as a planned, structured, and repetitive physical activity with a goal of maintaining or improving physical fitness.6
Physical activity is greatly reduced in people with MS, as documented in empirical studies7 and a metaanalysis.8 The meta-analysis, in particular, indicated that people living with MS overall were approximately 1 standard deviation less physically active than the general population of healthy adults,8 who, parenthetically, were largely sedentary.9 The reduction in physical activity was larger in those with a progressive compared with a relapsing clinical MS course,9 suggesting that disease severity is associated with physical inactivity. Recent evidence has indicated that physical activity in MS linearly declines over time, and fewer than 20% of individuals with MS meet current guidelines for moderateto-vigorous physical activity.7 Together, this evidence underscores a critical need and opportunity to improve walking mobility, symptoms, QOL, and participation among those with MS—if we are able to develop effective behavioral interventions that increase physical activity.10,11
Qualitative inquiries have been conducted to better elucidate the meaning, motivations, and benefits of physical activity and exercise among those with mild and moderate MS.12-16 These data have helped inform successful physical activity and exercise interventions.10,11 To date, only a few qualitative studies have been performed exploring the meanings, motivations, and benefits of physical activity in those with more advanced MS who are wheelchair users. These views have been primarily captured alongside those of people with milder forms of MS, with only one study specifically focused on wheelchair users who have MS.17 Accordingly, the perspectives of people who use wheelchairs cannot be easily differentiated from those of people who are not wheelchair users.
In these past studies, the facilitators that were identified included accessibility of facilities, appropriate professional support and self-regulatory strategies (eg, self-efficacy, goal-setting, and self-monitoring), social physical activity or exercise, and physical activity or exercise appropriate to one’s capabilities. Perceived barriers to physical activity and exercise included disease-specific obstacles (eg, weakness, fatigue, heat sensitivity, medication side effects), personal beliefs (eg, fear and lack of time and money), and lack of professional promotion or inaccessible facilities.12-18 The perceived benefits of exercise in those with MS have included symptom and functional improvement, and improvement in areas related to psychosocial factors (eg, enjoyment of life and social participation).12-18 Empowerment and control are important benefits that have been acknowledged across the disability spectrum in MS,13,14,16-20 particularly as they can lead to feelings of self-management in relation to physical activity.
However, it is important to capture the unique meanings, motivations, and benefits of physical activity specifically in wheelchair users who have MS. More than 10% of people with MS will require mobility devices (eg, a wheelchair) within 10 to 15 years after MS diagnosis.21 Wheelchair use has a negative association with physical activity and exercise participation.22 Qualitative inquiry suggests that advancing MS affects daily life, which may influence the design and delivery of physical activity and exercise interventions for wheelchair users. Thus, further study of physical activity in people with advanced MS is vital.
The present study extends previous qualitative research by focusing on a nonambulatory group of individuals, namely wheelchair users who have MS (ie, advanced MS). Two questions were explored: 1) What are the everyday experiences and lifestyle management strategies of wheelchair users who have MS? 2) What are the meanings, motivations, and outcomes of physical activity and exercise for wheelchair users with MS? The first question helped to identify possible opportunities for accruing physical activity in the context of daily life. The second helped identify targets of an intervention for changing physical activity behaviors.
Methods
Study Design
Our basic qualitative research design included semistructured interviews with 15 people who had MS and were wheelchair users (dependence on manual or powered wheelchair for ≥80% of the day or ≥40 hours per week). Ethical approval was granted by a university institutional review board. All participants provided written informed consent along with a physician-confirmed verification of MS diagnosis.
Interpretation of qualitative data involves subjectivity and bias; therefore, eliminating the influence of the researchers’ views is impossible in qualitative research.23 We aimed to understand our personal experiences, expectations, and values, and to use this awareness productively as we coded the data and drew conclusions.
Our research team consisted exclusively of clinical researchers. Two of the five researchers (YCL and RWM) had a background in physical activity/exercise among people with MS. Of the two interviewers, one (YCL) had been an exercise trainer for three of the participants prior to the interviews, and another interviewer (IMR) was a wheelchair user. The interviewers’ experiences appeared to contribute to participants’ feeling more comfortable in sharing their experiences and perspectives.
Participant Recruitment
We recruited a sample of people with MS who were wheelchair users. Participants were recruited from the Midwest region of the United States. Potential participants were informed of the study through 1) a recruitment letter sent to individuals in the North American Research Committee on Multiple Sclerosis study participation database living within 125 miles of the research site; 2) a recruitment phone call to individuals who had previously taken part in our research; or 3) presentations by our research staff at National Multiple Sclerosis Society meetings and events. Initially, 55 people with MS expressed interest in participation, and these people were contacted by members of the research team directly, who explained the study in greater detail. After this explanation, 12 were no longer interested, as they were unable to travel to the testing site or did not have the time to participate. Forty-three potential participants were then screened by telephone for the following inclusion criteria: 1) diagnosis of MS, 2) wheelchair user (defined as any individual who uses a mobility device or multiple mobility devices [power or manual] as a primary means of mobility for ≥80% of ambulation or ≥40 hours per week), 3) aged 18 to 64 years, and 4) stable health status for the past 3 months. We aimed to capture opinions on physical activity and exercise from a representative sample of wheelchair users who have MS.
Exclusion criteria were 1) being a wheelchair athlete, 2) orthopedic upper-extremity impairment, 3) selfreported history of cardiovascular or cardiopulmonary disease, and 4) pressure ulcers. Wheelchair athletes typically participate in more exercise than nonathletes, and those with cardiovascular or cardiopulmonary disease may require physician approval and specialized programs in order to undertake physical activity or exercise. A total of 21 individuals were excluded (14 participants did not use a wheelchair, 4 were undergoing change in symptoms or health status, and 3 were too old), leaving 22 potential participants. We conducted interviews with 15 of the 22 individuals, as we reached data saturation (ie, no new themes emerging relating to everyday [lifestyle management] experiences and the meaning of and motivations for physical activity and exercise).
Clinical and Lifestyle Demographics
When participants arrived in our laboratory, we provided further explanation and obtained informed consent. We administered a standardized survey form to capture basic background information on the participant’s demographic (age, sex, ethnicity) and clinical (type of MS and years since diagnosis) characteristics. We also collected information related to exercise levels (number of sessions per week; we did not provide participants with any definition of exercise at this stage, as doing so may have influenced our interview discussions), mobility aids owned, primary-care assistance in the home (independent, family member, or paid personalcare attendant), main transport mechanism (chauffeured, independent, or public transport), and contact with health-care professionals.
Interview Protocol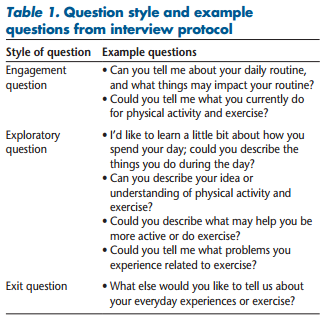
We conducted the interviews in a quiet office using a standardized semistructured interview schedule. The formal interview questions were based on the qualitative literature on social participation, everyday experiences, lifestyle behavior, and physical activity and exercise in MS. Interview questions included engagement questions, exploratory questions, and exit questions (Table 1). The responses to these standard questions were explored further for clarification and depth of inquiry. The interviews lasted on average 45 minutes and always opened with the quantitative survey before moving into the areas of everyday experiences, physical activity, and exercise. Interviews were led by one researcher (IMR), with additional questions added by YCL. The participant was the primary interviewee, but five participants were accompanied by caregivers (family member or personal-care attendant), who provided some input during the interviews. All participants received $20 for their participation.
Analysis of Data
The recorded interviews were transcribed verbatim and read multiple times by the two interviewing researchers (YCL and IMR) and analyzed based on standard guidelines.24 We began analyzing our data concurrently as new interviews were occurring. Using open coding, we analyzed one interview to develop themes, then put the findings aside before analyzing the next. This process was repeated for the first ten interviews. To do this, each researcher independently coded the transcriptions line by line and created notes/topic areas from each interview. The researchers then met and discussed topic areas to generate key themes, with 26 different codes initially emerging from the interviews. We then created a coding frame from these 26 codes, and the final five interviews were processed using this coding frame; the original ten interviews were reanalyzed using the coding frame. This permitted both inductive (data-driven) and deductive (concept-driven) analysis of the data. The 26 codes were then further refined and renamed to 18 codes of direct relevance to the research questions. Five subthemes emerged from these codes, which yielded two overall themes. This article reports on the findings related to 1) everyday experiences of people with MS who were wheelchair users and 2) participants’ views and experiences related to physical activity and exercise.
Strategies for Improving Trustworthiness
We used several strategies to improve the rigor of this study.24 Interview reliability was addressed by using a standardized semistructured interview script and having both interviewers present at all interviews. Prolonged engagement was achieved by continuing interviews until data saturation was achieved. Triangulation of our data source was done by intertwining results from our survey data (particularly current exercise participation, primary home caregiver, driving status, and health-care professionals seen) with the interview findings. Triangulation of our analysis was ensured, as transcript analysis was undertaken by two investigators separately before they met to discuss findings. Furthermore, we met frequently with our wider research team (LAR and RWM) to discuss our findings and analysis plans.
Results
Participant Characteristics
The study population was largely female (n = 12) and white (n = 13). The mean age of the participants was 52 (SD 8.8, median 54) years. There was a similar distribution of married (n = 8) and single (n = 7) participants, and the majority were unemployed (n = 13). Clinically, participants reported having relapsing-remitting (n = 7), secondary progressive (n = 6), and primary progressive (n = 2) MS. Mean disease duration was 14.3 (SD 8.5, median 15) years. These descriptors plus wheelchair use (n = 11 powered wheelchair, n = 4 manual wheelchair) indicate that the sample was typical of an advanced MS population.
Data Analysis 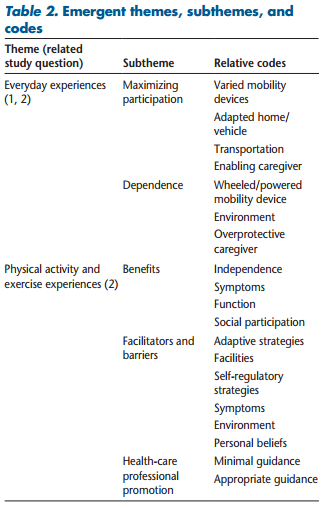
Interview analysis resulted in the emergence of two overall themes comprising five subthemes based on 19 codes (Table 2). The first theme, named “Everyday Experiences,” was primarily related to the first study question regarding the social experiences and lifestyle management strategies of participants. There were two subthemes related to “Everyday Experiences,” namely “Maximizing Participation” and “Dependence.” The second theme, named “Physical Activity and Exercise Experiences,” was principally related to the second research question regarding meanings, motivations, and outcomes of physical activity and exercise. There were three subthemes related to “Physical Activity and Exercise Experiences,” namely “Benefits,” “Facilitators and Barriers,” and “Health-Care Professional Promotion.”
Theme 1: Everyday Experiences
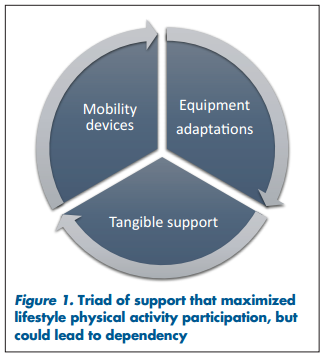
Maximizing Participation. Participants discussed ways in which they maximized participation in their home, in the community, and while undertaking social activities. Specifically, a triad of strategies was discussed (Figure 1). Participants owned different mobility devices (eg, canes, walker, wheelchair or powered wheelchair), used equipment adaptations (ie, home adaptations, home assistive devices, transport alterations), or accessed tangible support (eg, caregiver assistance for cooking, cleaning, or transport) to maximize physical activity participation. The participants were all wheelchair users, and many owned multiple mobility devices that were required to combat disability progression, symptom changes, and environmental hurdles: “I choose my mobility device based on space and energy. Inside my small house I use my walker, or sometimes I have to use forearm crutches in narrow doorways. Everything needs to be planned out, I don’t have room for my manual chair, so I leave it in the car. I need my wife’s help if I need that. Then if I go any great distance outside I need my powered chair” (Participant 4).
Participants had made adaptations around their home to make it easier for them to participate in everyday activities, for example, in the kitchen or bathroom. These equipment adaptations allowed them to maintain or regain independence despite their reduced mobility: “I have handrails in my hallway, a roll-in shower, and my house is on one level, it’s wonderful. My kitchen is super MS-friendly, I can reach both counters now, I have a stool, all around my house I can hold on for support, we even moved my bedroom downstairs” (Participant 5). Some participants had made adaptations to their private car that made it easier for them to use their own transportation, allowing them to remain independent and maximize participation in social activities: “I’ve a car with hand controls, it was scary at first, a little different. Now I can just go and pick friends up, or they can come to me. I can choose where I go, we will go shopping or wherever” (Participant 15).
 Many participants used the tangible support of a caregiver to help with many everyday tasks, which allowed them to participate in social activities. This caregiver was often either a spouse or another family member (n = 6) or a paid personal-care assistant (n = 3). Most participants (n = 9) did not drive; therefore, in order to participate in everyday or community activities they either were chauffeured in a private car or used public transportation. Participants recalled examples of the social activities they enjoyed and explained that they used the support of a caregiver to help them participate: “A lot of times I socialize where my son works, it’s a tavern. I use the bus to get me there, then he brings me home. Or, if I go out, like the other night I went out to eat with my cousin, they’ll help and come and pick me up” (Participant 5).
Many participants used the tangible support of a caregiver to help with many everyday tasks, which allowed them to participate in social activities. This caregiver was often either a spouse or another family member (n = 6) or a paid personal-care assistant (n = 3). Most participants (n = 9) did not drive; therefore, in order to participate in everyday or community activities they either were chauffeured in a private car or used public transportation. Participants recalled examples of the social activities they enjoyed and explained that they used the support of a caregiver to help them participate: “A lot of times I socialize where my son works, it’s a tavern. I use the bus to get me there, then he brings me home. Or, if I go out, like the other night I went out to eat with my cousin, they’ll help and come and pick me up” (Participant 5).
Participants recalled other examples of combining strategies from the triad of support, allowing them to maximize participation in everyday tasks. For example, by having help from a caregiver and making everyday equipment in their homes easily accessible, participants could cope with some of their MS symptoms better and feel like they could participate in normal family activities: “I still try to cook our dinner, not as much as before. I’m tired at the end of the day, so my husband helps. But I have everything positioned to make it easier to move in the kitchen, my husband helps me getting and planning everything we need” (Participant 9).
Dependence. The same triad that maximized participation in daily activities (ie, mobility devices, adaptations, and support) caused dependency and reduced opportunities to participate in physical activity. Participants described how they depended on mobility devices and tangible support throughout their everyday experiences. Many reported that relying on the support strategies of mobility devices (eg, using a powered wheelchair rather than a manual self-propelled wheelchair), caregivers, or adaptive equipment (eg, relying on a caregiver or lifting equipment to facilitate transfers rather than actively completing transfers) reduced their motivation for active movement (ie, lifestyle physical activity) in the everyday environment.
All of the participants gave examples suggesting that everyday life was more difficult now that they used a wheelchair. Many talked about the difficulties they had moving around their home and other environments, and stated that they felt they needed to conserve energy. To conserve energy, they planned tasks to minimize their level of effort: “Everything at home is really, really difficult. I plan out every single thing. If I’m going into the living room then you know I plan what I’m needing. I don’t want to get in there and realize there is something I need from the bedroom. It takes so long to go back” (Participant 4).
Some participants reported that as their disability had progressed they relied more heavily than before on assistance from a caregiver. For some participants, having to depend on other people caused frustration: “I have helpers who insist on taking care of everything. I used to cook all the time; I get very tired and Elaine [caregiver] now fixes me breakfast, lunch, and sometimes dinner. I’m not really happy about them doing everything, independence was always a big thing for me, and now the dependency on other people really bothers me” (Participant 3).
As a result of their use of a wheelchair and having decreased mobility, participants needed to plan and organize transportation in advance, and many needed to take special mobility equipment when traveling. Furthermore, they needed assistance from other people. These factors limited independent travel: “[When leaving the home to travel] I need my suitcase ramp, my powered scooter, my seated Rollator, and everything. Then I transfer into my car, but I can’t do that on my own. I always have to take someone with me” (Participant 14).
Problems using their mobility device in social spaces, often when external environments were not adapted appropriately, meant that participants were less likely to partake in the related activity, thus reducing the opportunity to accumulate lifestyle physical activity. Almost all the participants relayed examples of poorly adapted environments for wheelchair users, including smaller or older shops and restaurants: “Most places are accessible around town. The only place, my favorite café, I used to like to go there. It’s not handicap accessible that I can find, it has three steps to get in, so we don’t go. But most places are fairly accessible” (Participant 3). “Me and my wife are planning on seeing a movie soon, that’s accessible [for my wheelchair]. But for a restaurant beforehand I’ll only go if I know it’s accessible. I’ll always check if it is, and if not, or if it’s busy, I’ll not go” (Participant 5).
Theme 2: Physical Activity and Exercise Experiences
Our interest in the physical activity and exercise experience of wheelchair users who have MS led to exploration of areas related to physical activity and exercise. Without providing them with a formal definition, we asked participants to explain to us what physical activity and exercise were. The participants perceived physical activity to be part of everyday experiences such as chores or looking after their family, whereas exercise was seen as following a set of specific movements, using equipment and purposively choosing to make time to do the activity. Such informal definitions of physical activity and exercise mirror our formal definitions (ie, physical activity: “any bodily movement produced by skeletal muscles resulting in energy expenditure”; exercise: “a planned, structured and repetitive physical activity with a goal of maintaining or improving physical fitness”6 ): “I consider exercise a deliberate thing, you know stretching, jogging, lifting weights. But physical activity is basically anything that gets me off my butt and doing something, anything” (Participant 4). “Exercise is actually the intensity, the harder you do something, but physical activity is just what you do every day, walking or anything around the house” (Participant 5). The discussion moved on to participants providing stories and examples of the consequences (ie, benefits and adverse effects) and determinants (ie, facilitators and barriers) related to participating in physical activity and exercise.
Positive Benefits. The majority (n = 11) of participants undertook exercise at least once a week. Many benefits from physical activity and exercise were acknowledged by all participants (Figure 2), and ultimately exercise was perceived to be a self-management tool. Participants provided examples of the improvements physical activity and exercise brought to their physical symptoms (ie, fatigue, strength, mobility). They also discussed how this led to improvement in their general functioning and reduced fall frequency: “I move better and I feel better when I exercise; my legs and my arms are better, I have a big car so it takes strength to turn the steering wheel. Getting on and off the toilet is a huge thing for my arms too” (Participant 15).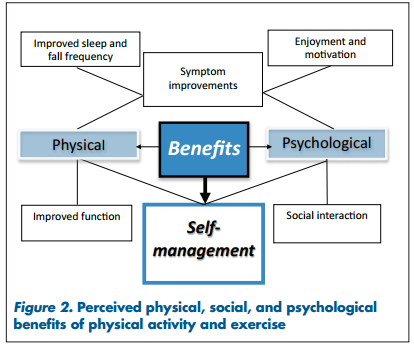
Participants also discussed the psychological benefits of physical activity and exercise. These included improvement in mood and increased enjoyment, motivation, and social participation: “Being with others is good, you bounce off one another, it’s important for motivation” (Participant 14). Although postexercise fatigue was noted by some, it was often discussed within the context of “feeling a healthy tiredness.” Ultimately, no participant reported any physical or psychological adverse consequence of physical activity or exercise.
The adverse consequences (ie, side effects) of MS pharmacologic interventions were discussed by some. Participants compared the benefits of physical activity with the adverse side effects of medication: “I want to exercise because I have absolutely zero faith in the medicine, I think it is overrated, it only works for a third of people and it makes you feel like crap, so I don’t take it. I’ve read lots of things about exercise and diet [for MS] on the Internet, and I think they are the only two good things I’ve ever read about treating MS” (Participant 4).
Current exercisers acknowledged that exercise helped them take control of their MS. Indeed, many participants provided examples of how exercise can be used as a tool and an opportunity to self-manage their disease. Furthermore, they related that while starting to participate in exercise might have been difficult, they felt it was important to overcome any barriers preventing them from participating: “Exercise is important; I think I need it; the exercise helps keep me from progressing. I think it is something I neglected a few years ago. I think that if 5 years ago I had been exercising I wouldn’t be in a wheelchair right now. I need to help myself now” (Participant 8). “I decided I wanted to do exercise because I want to walk my son down the aisle. The opportunity [to participate in an exercise program] came up and I thought, well I might as well do it. Then the more exercise I did, the more I could see I was getting better, my smaller goals are just to be able to walk more, I need to do it as I don’t like being in a wheelchair all the time” (Participant 5).
Facilitators and Barriers. Facilitators of lifestyle physical activity and exercise participation were discussed by all participants, along with barriers to these behaviors. As depicted in Figure 3, the decision to change the degree of physical activity or exercise participation was based on balancing facilitators and barriers. Adaptive strategies (eg, adapted exercise, accessible equipment, and appropriate temperatures) were suggested as a means to manage and overcome MS symptom–related barriers to physical activity and exercise. Participants suggested that appropriate facilities (ie, accessible venues, including the participant’s own home) would facilitate participation and overcome environmental barriers; they gave examples of good facilities and exercise equipment they had previously used: “If I could design my own exercise environment, it would be like the gym at the rehab institute. Their gym is amazing, they have a bike you can easily get on, and you peddle and pull back, it’s amazing. Everything can be broken down so that if I didn’t want to get out of my chair I could pull up to it, and just start exercising. It’s convenient, I can do what I want, as much and as often as I want” (Participant 11). 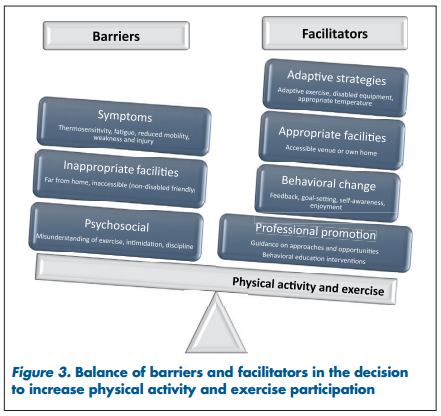
Participants discussed positive behavioral factors (ie, psychosocial facilitators) that they felt helped them become more physically active and exercise. These included receiving positive feedback from others, motivational goal-setting, increasing self-awareness of improvement, and following an enjoyable program. Participants provided examples of how these factors helped them to overcome negative personal beliefs (ie, a misunderstanding of what physical activity and exercise is, intimidation, and a lack of discipline) related to physical activity and exercise: “My biggest fear [when starting a new physical activity or exercise intervention] would be not being able to do the exercise. Nine months ago I didn’t think I could do the treadmill. I found a place that I could do my exercise, you’ve got to have someone there telling me what I’m doing, right or wrong. It’s good to have a trainer to talk to, distracting me, because before you know it you’re done; that’s 20 minutes on the treadmill done” (Participant 5).
Many participants discussed the social aspect of physical activity and exercise; examples of such social facilitators included spending time with peers and making friends, and the guiding role physical activity professionals play when wheelchair users with MS participate in physical activity and exercise: “It’s motivating being around other people, and I would want to have someone there to help me, someone to tell me and make sure I am doing the right thing” (Participant 7).
Professional Promotion. The potential guiding role of healthcare professionals was discussed by participants; it emerged that interactions with health-care professionals were important with regard to participants’ opinions and knowledge of physical activity and exercise. Participants stated that health-care professionals are one important source of information on physical activity and exercise. Moreover, promotion by health-care providers played a role in the decision to increase lifestyle physical activity and exercise (and thus is included in Figure 3). Participants’ primary point of contact with the health-care system was either a general practitioner or a neurologist, and many also had contact with a physical therapist. Most participants’ health-care professionals were generally in favor of exercise. Participants provided examples of good professional promotion of physical activity and exercise; these positive experiences seemed to incorporate self-regulatory strategies and were perceived to guide and advise the participant on approaches, opportunities, and actions to increase physical activity and exercise. These insights were provided by participants who reported that they were active exercisers: “They [participant’s healthcare professional, does not specify which] tell me every thing with MS is controlled by physical activity, they just want you to keep moving, whatever it takes, however you do it. Do it. A few years ago I went to an MS talk and an MS exercise trainer was there. She told us you have to keep doing physical activity, maintain and exercise your muscles. But she told us not to overdo it, she knew we would get tired, and end up on the couch for the rest of the day” (Participant 14). “I’m doing an exercise program here [university MS exercise program with an exercise trainer highly knowledgeable about exercise for MS], and I think doing this program is help ing me with goals. Like I know how many minutes or so that I’ve to go, or how many reps. I’m using the bus to get here too, it’s making me think I can maybe use the bus to get to other places too. My goal is to be able to get to church on the bus” (Participant 3).
Some participants reported that not all interactions with health-care providers were as positive; often the health-care provider gave little prescriptive or practical advice. Participants provided specific examples of times when they had encountered minimal professional awareness or promotion of physical activity and exercise: “My doctors tell me I should do it [exercise], my regular doctor tells me I should do it six times a week, but I don’t have anywhere to do it that often. He doesn’t give me any ideas where I can exercise” (Participant 5). “They [health-care professionals] have told me nothing really. The neurologist said by all means keep exercising, but gave nothing specific. I’ve only had three visits to the physical therapist and we only worked on my lower body” (Participant 15).
A small number of participants recalled that some of their health-care providers did not advocate exercise, cautioned them against certain exercises, or seemed unknowledgeable about exercise for those with advanced MS. These insights came from participants who reported that they rarely exercised: “Earlier on, before she progressed she did go to some therapy, some exercises, but there’s nothing now [that she has more advanced symptoms], they [the therapists and doctors] don’t know what else to do” (Participant 6’s husband). “They [the therapists and doctors] really don’t know as much as they should, they tell me to read books [fiction stories] and watch my programs [television movies]” (Participant 6). “I went to see a physical therapist at the Spine Institute and he basically told me, ‘Here’s exercise I give healthy people. I don’t know if I can do anything since you’re so bad off with your MS, but we’ll give it a try,’ but he did give me things to do” (Participant 4).
Discussion
Increasing physical activity and exercise is a critical component of MS care and a salient strategy in patient self-management.5,25 Historically, people with advanced MS (eg, wheelchair users) have been poorly represented in physical activity and exercise research.2 This qualitative work sought to elucidate the meanings, motivations, and benefits of physical activity and exercise among people with advanced MS who are wheelchair users. The study yielded rich data on life-style, physical activity, and exercise participation issues perceived by those with advanced MS. Two main themes were identified: everyday life experiences, and perceived benefits of physical activity and exercise participation.
Findings on our first theme offered insight into lifestyle physical activity opportunities. Participants used a triad of support strategies (mobility devices, equipment adaptations, and tangible support) to maximize participation in everyday life. Mobility problems were universal and resulted in participants’ need to use varied and multiple mobility devices, consistent with previous findings.26 Similar to the findings of past studies, tangible support was common27,28 yet counterproductive with regard to lifestyle physical activity.29 New findings emerged on equipment adaptations around the home and in personal vehicles that allow people with advanced MS to undertake everyday tasks. The efficacy of such adaptations should be assessed in future research.
Previous research has indicated that those with more progressive forms of MS are especially inactive.9 Our data provide insight into potential interventions to increase physical activity opportunities in wheelchair users with MS. Each area in the triad of support presents an opportunity to accumulate lifestyle physical activity and maximize self-management: for example, the use of wheeled mobility aids that require self-propulsion, the use of modified vehicles and driver training to allow independent driving, and behavioral interventions to encourage and facilitate self-management of everyday tasks.
Findings on the second theme, perceived consequences of physical activity and exercise participation, were consistent with previously recorded discussions among people across the MS disease spectrum12-18 and with the empirical evidence.2 The perceived benefits include improved mobility, function, strength, mood, fatigue levels, and overall QOL. In our study exercise was perceived to offer control and empowerment, echoing the findings of previous qualitative studies.13,14,16-20 Moreover, the potential for exercise to facilitate disease self-management was acknowledged at a consensus conference on important areas in MS care.4 However, the relationship between physical activity and exercise and self-management in those with advanced MS has not been subjected to robust quantitative analysis. Researchers must now confirm quantitative evidence of the role physical activity and exercise interventions play in disease self-management among people with advanced MS. No adverse consequences beyond “healthy fatigue” were perceived by our participants. Indeed, participants contrasted the positive consequences of physical activity and exercise with the adverse side effects of MS pharmacologic interventions.
Our participants perceived similar barriers to exercise as others with MS,18,30 namely, MS symptoms, inaccessible environments, and negative personal beliefs about physical activity and exercise. Key facilitators of increased physical activity and exercise include adaptive strategies such as adapted physical activities and exercise performed in an accessible environment with an appropriate temperature. Interventions should also contain behavioral change components to encourage initiation and maintenance of lifestyle physical activity and exercise behaviors.
The current low levels of physical activity and exercise participation in those with advanced MS may result from the barriers outweighing the facilitators. Interventions to address this imbalance are essential to achieving comprehensive MS health care.4 Our results suggest that promotion of physical activity and exercise by MS health-care professionals is an important facilitator of such activity in people with advanced MS. Therefore, research is needed to discover the educational and service needs of MS health-care professionals that will enable them to effectively promote physical activity and exercise to their MS patients. This will improve patient selfmanagement and ultimately the health of people with advanced MS.
Some limitations of this study should be noted. First, our sample was purposive and specific to wheelchair users with MS, allowing us to capture and present the unique voice of those with advanced MS in relation to physical activity and exercise. Thus, the findings may not be applicable to other populations, including those who require less ambulation assistance as well as those who have higher levels of dependence. Second, the quality of the demographic, clinical, and lifestyle data (ie, exercise behavior and time spent ambulating) gathered limited our analysis; we recommend the future use of standardized outcomes to capture these data. Third, the majority of our participants were middle-aged, and different results might be found for people who are either younger or older. Finally, our results are subject to potential researcher confirmation bias; however, the clinical and real-life experiences of our research team added depth and insight to the overall analysis.
 Conclusion
Conclusion
Maintaining lifelong physical activity and exercise is important to maximize QOL in MS. However, people with MS are generally inactive. The results of this qualitative study confirm past research that found a desire to undertake more physical activity and exercise as well as to achieve independence and effective self-management among people with MS. Two priorities that will help them achieve these goals are targeting physical activity interventions specifically toward wheelchair users who have MS and educating health-care providers on the delivery and promotion of physical activity and exercise programs to those with advanced MS. These efforts may help people with MS gain the benefits of physical activity and exercise and thereby enhance their QOL.
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This work was supported by the National Multiple Sclerosis Society (grant IL0005).
References
1. Joy JE, Johnston RB Jr. Multiple Sclerosis: Current Status and Strategies for the Future. Washington, DC: National Academies Press; 2001.
2. Motl RW, Pilutti LA. The benefits of exercise training in multiple sclerosis. Natl Rev Neurol. 2012;8:487–497.
3. Ploughman M, Austin MW, Murdoch M, Kearney A, Godwin M, Stefanelli M. The path to self-management: a qualitative study involving older people with multiple sclerosis. Physiother Can. 2012;64:6–17.
4. Vollmer T, Benedict R, Bennett S, et al. Exercise as prescriptive therapy in multiple sclerosis: a consensus conference white paper. Int J MS Care. 2012;14:2–14.
5. Fraser R, Ehde D, Amtmann D, et al. Self-management for people with multiple sclerosis: Report from the First International Consensus Conference. Int J MS Care. 2013;15:99–106.
6. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126.
7. Klaren RE, Motl RW, Dlugonski D, Sandroff BM, Pilutti LA. Objectively quantified physical activity in persons with multiple sclerosis. Arch Phys Med Rehabil. 2013;94:2342–2348.
8. Motl RW, McAuley E, Snook EM. Physical activity and multiple sclerosis: a meta-analysis. Mult Scler. 2005;11:459–463.
9. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257.
10. Pilutti L, Dlugonski D, Sandroff B, Klaren R, Motl R. Randomized controlled trial of a behavioral intervention targeting symptoms and physical activity in multiple sclerosis. Mult Scler J. 2014;20:594–601.
11. Dlugonski D, Motl RW, Mohr DC, Sandroff BM. Internet-delivered behavioral intervention to increase physical activity in persons with multiple sclerosis: sustainability and secondary outcomes. Psychol Health Med. 2012;17:636–651.
12. Plow MA, Resnik L, Allen SM. Exploring physical activity behaviour of persons with multiple sclerosis: a qualitative pilot study. Disabil Rehabil. 2009;31:1652–1665.
13. Smith CM, Olson K, Hale LA, Baxter D, Schneiders AG. How does fatigue influence community-based exercise participation in people with multiple sclerosis? Disabil Rehabil. 2011;33:2362–2371.
14. Dlugonski D, Joyce RJ, Motl RW. Meanings, motivations, and strategies for engaging in physical activity among women with multiple sclerosis. Disabil Rehabil. 2012;34:2148–2157.
15. Giacobbi PR, Dietrich F, Larson R, White LJ. Exercise and quality of life in women with multiple sclerosis. Adapt Phys Act Q. 2012;29: 224–242.
16. Kasser S. Exercising with multiple sclerosis: insights into meaning and motivation. Adapt Phys Act Q. 2009;26:274–289.
17. Van der Linden ML, Bulley C, Geneen LJ, Hooper JE, Cowan P, Mercer TH. Pilates for people with multiple sclerosis who use a wheelchair: feasibility, efficacy and participant experiences. Disabil Rehabil. 2014;13:932–939.
18. Learmonth YC, Marshall-McKenna R, Paul L, Mattison P, Miller L. A qualitative exploration of the impact of a 12-week group exercise class for those moderately affected with multiple sclerosis. Disabil Rehabil. 2013;35:81–88.
19. Plow M, Finlayson M. A qualitative study exploring the usability of Nintendo Wii Fit among persons with multiple sclerosis. Occup Ther Int. 2014;21:21–32.
20. Smith CM, Hale LA, Olson K, Schneiders AG. How does exercise influence fatigue in people with multiple sclerosis? Disabil Rehabil. 2009;31:685–692.
21. Hirst C, Ingram G, Swingler R, Compston DS, Pickersgill T, Robertson NP. Change in disability in patients with multiple sclerosis: a 20-year prospective population-based analysis. J Neurol Neurosurg Psychiatry. 2008;79:1137–1143.
22. Best KL, Miller WC. Physical and leisure activity in older communitydwelling Canadians who use wheelchairs: a population study. J Aging Res. 2011;2011:147929.
23. Hammersley M, Atkinson P. Ethnography: Principles in Practice. 3rd ed. New York, NY: Routledge; 2007.
24. Creswell JW. Qualitative Inquiry and Research Design: Choosing Among Five Approaches. Los Angeles, CA: Sage Publications; 2012.
25. Fraser R, Johnson E, Ehde D, Bishop M. Patient Self-Management in Multiple Sclerosis [white paper]. Hackensack, NJ: Consortium of Multiple Sclerosis Centers; 2009.
26. Souza A, Kelleher A, Cooper R, Cooper RA, Iezzoni LI, Collins DM. Multiple sclerosis and mobility-related assistive technology: systematic review of literature. J Rehabil Res Dev. 2010;47:213–223.
27. Dunn J. Impact of mobility impairment on the burden of caregiving in individuals with multiple sclerosis. Expert Rev Pharmacoecon Outcomes Res. 2010;10:433–440.
28. Carton H, Loos R, Pacolet J, Versieck K, Vlietinck R. A quantitative study of unpaid caregiving in multiple sclerosis. Mult Scler. 2000;6:274–279.
29. Kayes NM, McPherson KM, Taylor D, Schlueter PJ, Kolt GS. Facilitators and barriers to engagement in physical activity for people with multiple sclerosis: a qualitative investigation. Disabil Rehabil. 2011;33:625–642.
30. Dodd KJ, Taylor NF, Shields N, Prasad D, McDonald E, Gillon A. Progressive resistance training did not improve walking but can improve muscle performance, quality of life and fatigue in adults with multiple sclerosis: a randomized controlled trial. Mult Scler. 2011;17: 1362–1374.


