Repair strategies for multiple sclerosis
Why is this important to me?
Substantial progress has been made in developing treatments for MS that target the immune system and reduce the relapse rate. However, these immunotherapies are not effective at halting permanent damage to your nervous system and the resulting permanent disability. Thus, treatment strategies that repair damage to the nervous system before permanent changes occur are critically important.
In MS, the immune system attacks and destroys myelin, the fatty substance that wraps around and protects nerve fibers. Nerve fibers that have lost their myelin do not function properly, leading to symptoms if you have MS. Nerve fibers that have been stripped of their myelin may also die, and this death of the nerve fibers and their nerve cells is generally considered irreversible. Thus, strategies aimed at repairing myelin damage and loss early in the disease course may prevent irreversible nerve cell death and permanent disability.
What is the objective of this study?
Researchers are actively investigating how myelin repair occurs, how to promote myelin repair, and how to visualize repair with imaging methods.
How does myelin repair occur?
- Electrical activity in the brain promotes myelin synthesis. Thus, some researchers believe that increasing neuronal activity in the brain may ultimately be useful for decreasing disability if you have MS.
- Myelin repair in the brain and spinal cord is performed by cells called oligodendrocytes, which are mature cells derived from a population of immature oligodendrocyte precursor cells. A second population of cells called neural progenitor cells can also generate mature oligodendrocytes. Myelin damage induces these immature pools of cells to migrate to areas of damage. Unfortunately, natural myelin repair is inefficient and incomplete, and therapies that increase myelin repair will likely be needed.
How can myelin repair be promoted?
- Researchers use several types of animal models to study myelin damage and repair.
- Researchers also use immature cells grown in a dish that have been designed to change color when treated with a compound that causes them to mature to a cell type that could make myelin.
- Animals with myelin damage or cells are treated with various molecules to identify one or more compounds that may be candidate drugs for promoting myelin repair.
- Some compounds that are being tested are already approved by the FDA for use in other diseases or conditions, which could speed up their possible use in humans with MS.
- Using these approaches, several candidate compounds that may promote myelin repair have been identified and are being tested in clinical trials in humans. Some examples are:
- Anti-Lingo-1 promotes myelin repair and is being tested in phase II clinical trials.
- Olesoxime may protect nerve cells and was recently tested in a phase I MS clinical trial.
- Clemastine is an FDA-approved anti-histamine that was recently tested in a phase II MS clinical trial for its ability to promote myelin repair.
- Siponimod may keep harmful immune cells out of the brain and is being tested in relapsing-remitting MS (phase II) and secondary progressive MS (phase III).
How can myelin repair be visualized?
- To determine if the above compounds and others promote myelin repair, methods to image myelin in patients—before, during, and after treatment—are needed.
- A major problem with current imaging methods such as MRI is that they are not specific to myelin.
- Researchers are actively working to overcome this problem using advanced imaging methods that may specifically show myelin in the future.
How did the authors study this issue?
The authors reviewed current considerations about myelin repair and animal and clinical studies testing myelin repair strategies.
| SHARE: | |||||
Original Article
Repair strategies for multiple sclerosis: challenges, achievements and perspectives
Bruno Stankoff; Janusz Joachim Jadasze; Hans-Peter Hartunge; Patrick Ku ̈rye; Bernard Zalc and Catherine Lubetzki
Current Opinion in Neurology
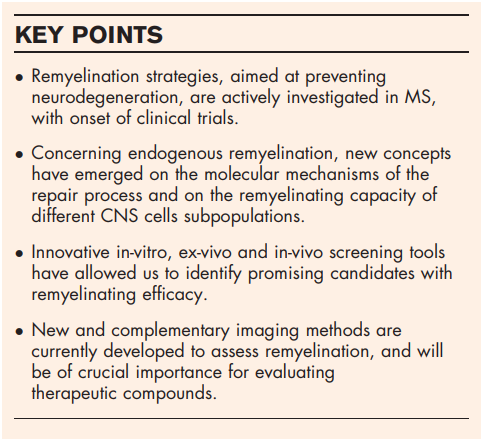
Purpose of review: Despite major progress in multiple sclerosis (MS) treatment, to date, accumulation of irreversible clinical disability is not sufficiently prevented with immunotherapies. In this context, repair strategies aimed at reducing axonal damage are becoming a very active field of preclinical and clinical research.
Recent findings: Improved understanding of the cellular and molecular mechanisms of myelin repair, together with the emergence of new therapeutic candidates are paving the way for novel therapeutic strategies in MS. In parallel, there is a very active development of imaging methods to assess lesions ongoing remyelination that are crucially needed to evaluate therapeutic efficacy.
Summary: The current development of a very dynamic and multidisciplinary research on remyelination should accelerate the development of myelin repair strategies in MS, to prevent disability progression.
INTRODUCTION
Major progress has been achieved in the treatment of multiple sclerosis (MS) through the development of therapies targeting the immune system. Acting on different mechanisms/steps of the inflammatory component of the disease, these currently approved treatments reduce the relapse rate, with different efficiency and safety profiles [1–3]. However, there is little if any evidence on the efficacy of these drugs during the progressive phase of the disease [4–6]. Accumulation of irreversible clinical disability during this progressive phase mostly relates to irreversible neuronal/axonal damage and loss [7–10], which occurs early in disease evolution, before becoming clinically eloquent years later, after reaching clinical threshold.
Preventing neurodegeneration is therefore a major challenge in MS, to prevent disability progression. This can be achieved through the development of neuroprotective drugs, which currently is an active, even though to date disappointing, area of research in different neurodegenerative diseases. Alternatively, promoting remyelination might favor neuronal protection, as suggested by studies in different experimental models, on the one hand, and by analysis of demyelinated and remyelinated lesion from postmortem MS brain, on the other [11–13].
Recent years have been fruitful for our better understanding of cellular and molecular mechanisms of the remyelination process, using a wide variety of demyelination/remyelination models, and this has resulted in the identification of several therapeutic targets and recent development of different preclinical and, very recently, to early phases of clinical remyelinating strategies. Although these recent translational developments are highly interesting, repair strategies are facing one major obstacle which is the lack of suitable markers of neuroprotection (or damage) and remyelination (or persisting demyelination) to evaluate therapeutic efficacy. In this respect, the current emergence of promising imaging markers represents a crucial advance that will impact the evaluation of repair strategies and design of therapeutic trials.
In this article, we will first review some recent and promising findings on the mechanisms of myelination and endogenous myelin repair, which illuminate our understanding of the repair process and might impact the development of therapeutic strategies. Then we will make an overview of the current and very active development of new screening tools and resulting early clinical trials. For the sake of space, we will focus on strategies aimed at promoting endogenous myelin repair, without addressing the potential value of exogenous remyelination strategies through grafts. Finally, we will address the usefulness of new imaging methods to assess de/remyelination and how these new methods might influence therapeutic trials design in MS.
MECHANISMS OF ENDOGENOUS REPAIR
We will focus on two types of results which modify our understanding of the repair process and might impact therapeutic strategies.
Is the active brain able to stimulate repair?
Whether neuronal activity impacts repair capacity in the central nervous system (CNS) regained major interest recently. Indeed, the influence of electrical activity on myelination capacity was addressed long ago [14], using different neurotoxins acting on voltage dependent sodium channels and either blocking, like tetrodotoxin, or stimulating, like alpha scorpion toxin, neuronal electrical activity. By showing that silencing electrical activity reduces myelination without affecting oligodendroglial numbers, and that increased activity results in increased myelination, this study demonstrated for the first time the key role of electrical activity in the myelination process. It added new insight into the observations made decades ago on the influence of light on optic nerve myelination, showing retarded myelination in mice reared in darkness, and accelerated myelination induced by artificial eye opening in the rabbit [15,16]. After several years of ‘electrical silence’, these results were further confirmed and extended with the identification of adenosine, released from astrocytes [17], then glutamate, released along axons as molecular mediators of activity dependent myelination [18,19& ]. Using the zebrafish model, it was demonstrated that neuronal activity regulates myelin sheath production by individual oligodendrocytes in a synaptic vesicle release dependent manner [20& ]. Alternatively, the influence of neuronal activity for biased axon selection was suggested [21]. The influence of electrical activity was further addressed in vivo, using optogenetic stimulation of the murine unilateral premotor cortex, allowing us to demonstrate not only that blue light-induced neuronal activity promotes oligodendrogenesis and increases myelination, but also that premotor cortex stimulation results in behavioural improvement, quantified on swing speed of the correlate forelimb during normal gait [22&&]. This result opens new perspective on the potential functional benefit of brain activity. Finally, the relevance of this mechanism was addressed in a remyelination model in the rat, showing that blockade of electrical activity results in reduced remyelination, an effect which was attributed to neuronal activity-induced glutamate release at the neuron/oligodendrocyte precursor cells (OPCs) synapse, acting on OPCs differentiation [23].
Taken together, and although the models and interpretation differ (notably the debate on synaptic versus extra synaptic mechanism), these very important findings extend recent discoveries that social experiences and experimentally altered neuronal activity can influence myelin plasticity [24,25], hence have the potential to influence a functional outcome. Even if the clinical translation is still far, these data, which bring a novel insight into the mechanisms of myelination plasticity, are paving the way for new therapeutic development in which neuronal activity is a target to promote disability improvement.
What are the cells achieving remyelination in the adult brain?
Remyelination in the CNS has been shown several years ago to be achieved by parenchymal oligodendrocyte precursor cells (pOPCs), which persist in the adult CNS, representing up to 5% of the total cells in the brain. These cells are defined by the expression of platelet-derived growth factor receptor alpha (PDGF-Ra) and neural/glial antigen 2 proteoglycan. Fate mapping studies have demonstrated that pOPCs are able to generate new oligodendrocytes that contribute to remyelination following demyelinating insults [26]. To gain an insight into their specific characteristics, our group recently showed, on pOPCs purified from a transgenic mouse line in which PDGF-Ra expressing cells are green fluorescent protein (GFP) positive, that the transcriptomic profile of adult OPCs is more similar to that of adult mature oligodendrocytes, that is, the oligodendroglial differentiated cells, than from neonatal OPCs [27]. Interestingly however, these pOPCs are not the only remyelinating cells of the adult brain. Previous reports in experimental models in which focal demyelination occurs adjacent to the subventricular zone (SVZ) and in postmortem tissue obtained from MS patients [28], had already suggested that after a demyelinating insult, oligodendrocytes might be generated from subventricular neural progenitor cells (NPCs). This has been further explored in a recent study in which fate mapping was used to trace NPCs and pOPCs in a model of cuprizone-induced demyelination. This study provides strong evidence that demyelination induces the migration of large numbers of NPCs and that NPC-derived oligodendrocytes are the major contributors of remyelination in the corpus callosum, notably in its rostral part. Interestingly, myelin sheaths produced by these NPC-derived oligodendrocytes are thicker than those produced by pOPCs, regardless of axon calibre, hence indistinguishable from untreated controls [29& ].
In this search for the identification of remyelinating cells, the potential role of mature oligodendrocytes, addressed long ago with conflicting results [30,31] was recently revisited. Using inducible transgenic mouse strains in which mature oligodendrocytes were prelabeled by the expression of GFP and a spinal cord focal demyelinating model, it was shown that mature oligodendrocytes did not proliferate nor migrate into the damaged area. This genetic fate mapping study therefore firmly establishes that mature oligodendrocytes do not normally contribute to remyelination, hence are not a promising target for regenerative therapy [32& ].
Taken together, these findings have important implications for our understanding of the repair process and the development of myelin repair therapies. In relation with this improved knowledge of the repair process, identification of compounds with remyelinating activity using newly developed screening tools recently became a highly active area of research.
DEVELOPMENT OF MYELIN REPAIR STRATEGIES
The tools
To test the repair efficiency of potential candidates the most commonly used animal model is experimental autoimmune encephalomyelitis (EAE) developed in rodent. The difficulty to predict the size and localization of the demyelinating lesions are a drawback of EAE. An alternative to EAE is the use of toxic-induced demyelinations. One frequently used model is feeding the animal with cuprizone, a copper chelator. The advantage of the cuprizone model is to limit the localization of the demyelination to the corpus callosum and superior cerebellar peduncle. To better define the localization and the size of the lesions, models using local injections of myelinotoxic agents such as lysolecithin or ethidium bromide are also often used. Despite their advantages and limitations, these rodent models are not adapted to screen large series of compounds, but rather as a semi-final in-vivo test of a handful of candidate molecules that have been preselected by more adapted high-throughput or medium-throughput screening tests.
Chemical libraries of large pharmaceutical companies comprise between 0.5 and 3 million compounds [33]. An alternative to screening large libraries of unknown chemicals is reprofiling (repurposing or repositioning) of collections of small molecules with validated biological and pharmacological activities, in which safety and effectiveness have been demonstrated in clinical trials and many of them are Food and Drug Administration (FDA)-approved or European Medicines Agency-approved for other indication than MS.
High content screens are being developed based on OPC stable lines (Oli-neu or CG4) engineered to turn on a fluorescent reporter (GFP, or mCherry) when driven towards a more mature oligodendrocyte [[34]; Nait-Oumesmar, personal communication]. Other tests, more tedious, are based on immunolabeling of primary cultures of OPCs with antibodies detecting molecules expressed by mature oligodendrocytes (myelin basic protein or myelinoligodendrocyte glycoprotein being prime marker candidates). A library of 727 FDA-approved drugs has been tested on mouse pluripotent epiblast stem cell-derived OPCs to promote differentiation into mature oligodendrocytes [35].
To test final maturation of OPCs into myelinating oligodendrocytes some attempts are aimed at examining the wrapping potential of mature oligodendrocytes. This can be achieved on oligodendrocyte lineage cells co-cultured with neuron [36,37]. Although very powerful such co-cultures are more adequate to test candidate molecules and are not well suited for high-throughput formats [38]. More recently developed is a micropillar array device engineered with conical dimensions, which permits detection of concentric wrapping of oligodendrocyte processes similar to rings of myelin [39& ].
The myelination potential of lead compounds identified using these in-vitro tools needs to be confirmed in vivo. Before probing these candidates using the expensive and time-consuming rodent models, simple vertebrate experimental models have been developed, taking advantage of the transparency of their embryo. A novel screening platform for identifying potential remyelination-promoting compounds and for further filtering those that need not be investigated further has been developed using zebrafish larvae [40]. A Xenopus laevis transgenic line has also been developed allowing conditional ablation of myelinating oligodendrocytes. After completion of demyelination spontaneous remyelination occurs. Remyelination can be dramatically accelerated by adding drugs to be tested in the swimming water of the tadpoles. This X. laevis transgenic line constitutes a new and robust medium-throughput screening platform for myelin repair therapeutics in demyelinating diseases [41,42].
SOME OF THE CANDIDATES
Several promyelinating candidates have been proposed that could potentially be applied to MS. Here we report few examples (not an exhaustive review) and other therapeutic developments that are described in the article by Jadasz et al. (pp. 205–212) in this issue of Current Opinion in Neurology. Surprisingly enough, among the most efficacious, their mode of action is apparently very different. The most advanced candidate is antiLingo-1, an antibody directed against Lingo-1 protein [43]. The rationale for anti-Lingo-1 therapy is based on the observation that Lingo-1 protein inhibits the production of myelin, therefore antagonizing Lingo-1 should promote remyelination. Anti-Lingo-1 has performed well in animal models and is now in phase 2, as described in the article by Jadasz et al. (pp. 205–212), olesoxime (phase 1) is a cholesterol-oxime compound belonging to the family of mitochondrial pore modulators [44]; benzatropine (no ongoing clinical trial) is a selective M1 muscarinic acetylcholine receptor antagonist [45]; clemastine (phase 2) is a selective histamine H1 antagonist, binding to the histamine H1 receptor [39& ]; siponimod (phase 2 in relapsing–remitting form of MS; phase 3 in secondary progressive MS) is a sphingosine-1-phosphate ligand with an affinity to S1P1 and S1P5 receptors [42]. Using a repurposing strategy, two drugs, miconazole (an antifungic) and clobetasol (a glucocorticoid used in eczema), have been shown to be effective in promoting precocious myelination in organotypic cerebellar slice cultures, and in vivo in early postnatal mouse pups [35]. So far it is not clear whether the remyelination potency of these candidate drugs is mediated by acting directly on the oligodendrocyte cell lineage or on the microglial environment or both. This remains to be established and is an important issue because it may reorient notably future therapeutic developments aimed at favouring myelin repair in MS.
Taken together, these multiple tools and potential therapeutic hits leading to the onset of clinical trials in MS patients have profoundly modified our views on myelin repair strategy, which now becomes an active field for translation. In this context, developing markers of myelin repair is a crucial need for designing clinical trials assessing drugs with potential remyelinating capacity.
ASSESSING REMYELINATING LESIONS IN VIVO BY IMAGING
As the pathophysiology of demyelinating diseases such as MS involves multiple mechanisms such as inflammation, oedema, blood brain barrier leakage, demyelination and neuroaxonal damage, a great specificity towards myelin is required in order to quantify remyelination in vivo. Although some conventional MRI metrics, derived from T1 or proton density sequences, were reported to sensitively capture MS lesion recovery [46], they are generally considered as not sufficiently specific for myelin.
Magnetization transfer imaging (MTI), that allows us to assess the proton pool linked to macromolecule, was proposed as a measure of myelin content because of the overwhelming contribution of myelin to the macromolecules involved in the magnetization transfer phenomenon. However magnetization transfer ratio (MTR) changes in brain lesions could be influenced by water content and inflammation, especially in acute and sub-acute lesions associated with a blood brain barrier breakdown [47]. To minimize this limitation a method based on the segmentation of focal areas of MTR decrease was developed to assess longitudinally myelin dynamics in the damaged white matter, and patients with a greater MTR recovery showed a better clinical outcome [48]. In patients with MS the ability of brain white matter lesions MTR to recover trended to a decrease with time, becoming less pronounced during adolescence and adulthood in the case of paediatric MS [49]. However, recovering lesions could also be identified in the brain of patients with progressive MS, whereas they appeared more frequently in previously lesional tissue [50]. MTR has also been shown to be sensitive to cortical lesion and a methodology to assess cortical demyelination at the individual level has been developed [51]. Overall, although being probably the most popular MRI technique to approach the assessment of myelin content, to date the specificity of MTI for myelin is still suboptimal [47,52]. Although still technically challenging, quantitative MTI could provide a better specificity towards myelin, as recently shown in the mouse cuprizone model [53].
The multicomponent T2 analysis of spin echo data, by focusing on the short T2 peak, has been proposed to extract the myelin water fraction (MWF), which likely corresponds to water trapped within the myelin bilayer [54]. As the reproducibility of MWF measure has been questioned, using a region of interest analysis strategy a voxel-based analysis is recommended [55]. Few longitudinal data on lesional MWF are available, indicating that some changes compatible with remyelination could be identified in a 6-month time frame [56], but with a greater variability than using MTI [57]. Several adaptations of the concept were recently developed aimed at shortening acquisition times, covering the whole brain and increasing sensitivity, with some promising results in MS [58–61], but their preserved specificity towards myelin still await to be proven.
A decrease in radial diffusivity over time on diffusion weighted images compatible with remyelination has been described in MS lesions [62]. However, the measure of radial diffusivity is not yet specific for myelin content as it can be significantly influenced by axonal pathology, inflammation, oedema and crossing fibers at the microstructural level. Recent optimizations of diffusion weighted imaging could provide more specific tools for the myelin compartment. The application of diffusion basis spectral imaging, by modelling diffusion weighted signal as a linear combination of multiple tensors, discriminating between the anisotropic fibre component and a full range of isotropic components, either restricted (and related to cell infiltration) or unrestricted (and related to oedema), was shown to allow differentiation of inflammation and oedema, from axonal and myelin damage in the cuprizone mice model [63& ]. Diffusion kurtosis imaging, an extension of diffusion tensor imaging that provides metrics of diffusional non-Gaussianity, could also generate quantitative measures sensitive to myelin changes in the cuprizone animal models [64,65] with preliminary promising results obtained in MS [66].
A specific approach for myelin imaging could be achieved using positron emission tomography (PET). The first myelin radiotracer identified was the stilbene derivative, 1,4-bis(p-aminostyryl)- 2-methoxy benzene, also named BMB [67], that has recently been shown to interact directly with myelin basic protein [68]. A similar affinity for CNS myelin was reported for several other stilbene Congo red derivatives, allowing to monitor myelin dynamics in dysmyelinating and demyelinating models [69–71]. On the basis of a common target expressed in amyloid plaques and myelin, the thioflavin T derivative [11C]-2-(40 -methylaminophenyl)-6-hydroxybenzothiazole ([11C]-PIB) was also shown to stain myelin providing an opportunity to quantify myelin content changes in MS [72]. A pilot [11C]-PIB PET imaging study was therefore performed in MS and an noninvasive quantification method for the dynamic acquisitions was developed and applied [73]. The individual remyelination potential of patients with MS showed a great heterogeneity, and was highly correlated with neurological disability [74&&]. Therefore, monitoring myelin dynamics by PET could be a added value to stratify patients depending on their repair ability, and to specifically quantify myelin repair in early therapeutic trials of promyelinating compounds. There is a need for fluorinated compounds that would allow a more widespread dissemination to this technique, and emerging fluorinated amyloid tracers might be of interest as reported in a preliminary study [75].
Sample size estimations have been made to quantify therapeutic effects on brain lesions recovery using either conventional or MTI based metrics, emphasizing that groups of 10–70 patients could allow the detection of therapeutic effects with an acceptable power [46,48,76].
CONCLUSION
Favouring remyelination in MS is becoming the next frontier. In this context, our growing understanding of the repair process, combined with identification of promising therapeutic candidates and development of novel imaging tools will result in the onset of a new era of therapeutic trials, aimed at preventing demyelination-related axonal pathology leading to accumulation of disability. Even if optimal timing of these therapeutic interventions is still debatable, the fact that axonal pathology occurs early in disease evolution has to be taken into account. These repair strategies might therefore be better adapted to early MS and combined with anti-inflammatory treatment. They will need innovative trial design with a key role for imaging markers. Of note, two extensive reviews on myelin repair have recently been published [77,78].
ACKNOWLEDGEMENTS
None.
FINANCIAL SUPPORT AND SPONSORSHIP
Research on the subject of myelin repair in the French laboratory was supported by INSERM, the French MS research foundation ARSEP, the program ‘Investissements d’Avenir’ ANR-10-IAIHU-06, a grant from ‘Investissement d’Avenir – ANR-11-INBS-0011 – NeurATRIS’, and ANR grants STEMIMUS to C.L. and OLGA to B.Z. Research on the subject of myelin repair in the German laboratory is supported by the German Research Council (DFG: SPP1757, KU1934/5-1), the Christiane and Claudia Hempel Foundation for clinical stem cell research and the French societies ARSEP and AFM. The MS Center at the Department of Neurology is supported in part by the Walter and Ilse Rose Foundation and the James and Elisabeth Cloppenburg, Peek and Cloppenburg Du¨sseldorf Foundation.
CONFLICTS OF INTEREST
C.L. has received honoraria from Roche, Biogen, Genzyme, Novartis and participated to Vertex advisory board. B.Z. has received research grants from Novartis and EMD Serono. B.S. received honoraria from Biogen, Teva, Novartis, Genzyme, and research support from Genzyme and Merck-Serono. J.J. reports no conflict of interest. H.-P.H. received compensation for consultancy and speaking from Biogen, GeNeuro, Genzyme, MerckSerono, Novartis, Octapharma, Opexa, Receptos, Roche, Teva, and Sanofis. P.K. received compensation for consultancy and/or speaking from Novartis, Baxter, GeNeuro and Biogen – all with approval by the Rector of Heinrich-Heine-University.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
& of special interest
&& of outstanding interest
1. Oh J, O’Connor PW. Established disease-modifying treatments in relapsingremitting multiple sclerosis. Curr Opin Neurol 2015; 28:220–229.
2. Ontaneda D, Fox RJ, Chataway J. Clinical trials in progressive multiple sclerosis: lessons learned and future perspectives. Lancet Neurol 2015; 14:208–223.
3. Ransohoff RM, Hafler DA, Lucchinetti CF. Multiple sclerosis – a quiet revolution. Nat Rev Neurol 2015; 11:134–142.
4. Shirani A, Okuda DT, Stu¨ ve O. Therapeutic advances and future prospects in progressive forms of multiple sclerosis. Neurotherapeutics 2016; 13:58– 69.
5. Salvetti M, Landsman D, Schwarz-Lam P, et al. Progressive MS: from pathophysiology to drug discovery. Mult Scler 2015; 11:1376–1384.
6. Ontaneda D, Fox RJ. Progressive multiple sclerosis. Curr Opin Neurol 2015; 28:237–243.
7. Mahad DH, Trapp BD, Lassmann H. Pathological mechanisms in progressive multiple sclerosis. Lancet Neurol 2015; 14:183–193.
8. Campbell GR, Worrall JT, Mahad DJ. The central role of mitochondria in axonal degeneration in multiple sclerosis. Mult Scler 2014; 20:1806–1813.
9. Friese MA, Schattling B, Fugger L. Mechanisms of neurodegeneration and axonal dysfunction in multiple sclerosis. Nat Rev Neurol 2014; 10:225–238.
10. Criste G, Trapp B, Dutta R. Axonal loss in multiple sclerosis: causes and mechanisms. Handb Clin Neurol 2014; 122:101–113.
11. Hagemeier K, Bru¨ck W, Kuhlmann T. Multiple sclerosis – remyelination failure as a cause of disease progression. Histol Histopathol 2012; 27:277–287.
12. Kornek B, Storch MK, Weissert R, et al. Multiple sclerosis and chronic autoimmune encephalomyelitis: a comparative quantitative study of axonal injury in active, inactive, and remyelinated lesions. Am J Pathol 2000; 157:267–276.
13. Irvine KA, Blakemore WF. Remyelination protects axons from demyelinationassociated axon degeneration. Brain 2008; 131:1464–1477.
14. Demerens C, Stankoff B, Logak M, et al. Induction of myelination in the central nervous system by electrical activity. Proc Natl Acad Sci U S A 1996; 93:9887–9892.
15. Gyllensten L, Malmfors T. Myelinization of the optic nerve and its dependence on visual function. A quantitative investigation in mice. J Embryol Exp Morphol 1963; 11:255–266.
16. Tauber H, Waehneldt TV, Neuhoff V. Myelination in rabbit optic nerves is accelerated by artificial eye opening. Neurosci Lett 1980; 16:235–238.
17. Stevens B, Porta S, Haak LL, et al. Adenosine: a neuron-glial transmitter promoting myelination in the CNS in response to action potentials. Neuron 2002; 36:855–868.
18. Wake H, Lee PR, Fields RD. Control of local protein synthesis and initial events in myelination by action potentials. Science 2011; 333:1647–1651.
19. & Wake H, Ortiz FC, Woo DH, et al. Nonsynaptic junctions on myelinating glia promote preferential myelination of electrically active axons. Nat Commun 2015; 6:7844. Combining murine co-cultures of oligodendrocyte progenitor cells and dorsal root ganglia neurons, calcium imaging and electrophysiology, this study shows that oligodendrocytes preferentially myelinate electrically active axons, through a mechanism dependent of non-synaptic vesicular release of glutamate.
20. & Mensch S, Baraban M, Almeida R, et al. Synaptic vesicle release regulates myelin sheath number of individual oligodendrocytes in vivo. Nat Neurosci 2015; 18:628–630. Using a zebrafish model, which allows to visualize myelination in live animals, this study shows that tetanus toxin-induced abrogation of synaptic vesicle release reduces myelination, and that this effect was related to reduced myelin sheath number per oligodendrocytes. In contrast, increased neuronal activity promotes myelin sheath production per individual oligodendrocyte. This study provides a novel insight into the mechanism of activity-dependent regulation of myelin production.
21. Hines JH, Ravanelli AM, Schwindt R, et al. Neuronal activity biases axon selection for myelination in vivo. Nat Neurosci 2015; 18:683–689.
22. && Gibson EM, Purger D, Mount CW, et al. Neuronal activity promotes oligodendrogenesis and adaptive myelination in the mammalian brain. Science 2014; 344:1252304. In this study, neuronal activation is induced unilaterally in the premotor cortex by optogenetic stimulation in the adult murine CNS. This activation results in increased myelination, and related improved function in the corresponding limb. This is the first in-vivo demonstration that neuronal activity-induced myelin plasticity results in behavioural improvement.
23. Gautier HO, Evans KA, Volbracht K, et al. Neuronal activity regulates remyelination via glutamate signalling to oligodendrocyte progenitors. Nat Commun 2015; 6:8518.
24. McKenzie IA, Ohayon D, Li H, et al. Motor skill learning requires active central myelination. Science 2014; 346:318–322.
25. Makinodan M, Rosen KM, Ito S, et al. A critical period for social experiencedependent oligodendrocyte maturation and myelination. Science 2012; 337:1357–1360.
26. Zawadzka M, Rivers LE, Fancy SP, et al. CNS-resident glial progenitor/stem cells produce Schwann cells as well as oligodendrocytes during repair of CNS demyelination. Cell 2010; 6:578–590.
27. Moyon S, Dubessy AL, Aigrot MS, et al. Demyelination causes adult CNS progenitors to revert to an immature state and express immune cues that support their migration. J Neurosci 2015; 35:4–20.
28. Nait-Oumesmar B, Picard-Riera N, Kerninon C, et al. Activation of the subventricular zone in multiple sclerosis: evidence for early glial progenitors. Proc Natl Acad Sci U S A 2007; 104:4694–4699.
29. & Xing YL, Ro¨th PT, Stratton JA, et al. Adult neural precursors from the subventricular zone contribute significantly to oligodendrocyte regeneration and remyelination. J Neurosci 2014; 34:14128–14146. Using in-vivo genetic fate mapping, this study addresses the relative contribution, in the myelin repair process, of neural progenitor cells (located in the subventricular zone) versus parenchymal oligodendrocyte precursors cells (considered as the major cell type achieving remyelination). Neural progenitor cells were shown to have a major role in corpus callosum remyelination, therefore changing our views on the cells responsible for remyelination in the adult CNS.
30. Keirstead HS, Blakemore WF. Identification of postmitotic oligodendrocytes incapable of remyelination within the demyelinated adult spinal cord. J Neuropathol Exp Neurol 1997; 56:1191–1201. 31. Lubetzki C, Gansmu¨ller A, Lachapelle F, et al. Myelination by oligodendrocytes isolated from 4–6-week-old rat central nervous system and transplanted into newborn shiverer brain. J Neurol Sci 1988; 88:161–175.
32. & Crawford AH, Tripathi RB, Foerster S, et al. Preexisting mature oligodendrocytes do not contribute to remyelination following toxin-induced spinal cord demyelination. Am J Pathol 2016; 186:511–516. Previous studies claiming that oligodendrocytes are unable to contribute to remyelination can be questioned because of technical flaws in the approach taken. Here, this genetic fate mapping study in which reporter genes have been expressed exclusively within mature oligodendrocytes has provided more definitive evidence.
33. Macarron R, Banks MN, Bojanic D, et al. Impact of high-throughput screening in biomedical research. Nat Rev Drug Discov 2011; 10:188–195.
34. Joubert L, Foucault I, Sagot Y, et al. Chemical inducers and transcriptional markers of oligodendrocyte differentiation. J Neurosci Res 2010; 88:2546– 2557.
35. Najm FJ, Madhavan M, Zaremba A, et al. Drug-based modulation of endogenous stem cells promotes functional remyelination in vivo. Nature 2015; 522:216–220.
36. Lubetzki C, Demerens C, Anglade P, et al. Even in culture, oligodendrocytes myelinate solely axons. Proc Natl Acad Sci U S A 1993; 90:6820–6824.
37. Zhang H, Jarjour AA, Boyd A, et al. Central nervous system remyelination in culture – a tool for multiple sclerosis research. Exp Neurol 2011; 230:138– 148.
38. Demerens C, Stankoff B, Zalc B, et al. Eliprodil stimulates CNS myelination: new prospects for multiple sclerosis? Neurology 1999; 52:346–350.
39. & Mei F, Fancy SP, Shen YA, et al. Micropillar arrays as a high-throughput screening platform for therapeutics in multiple sclerosis. Nat Med 2014; 20:954–960. A novel device for reprofiling compounds with a potential for remyelination. Screening led to the identification of antihistaminic molecule clemastin as a potential therapeutic compound, and a phase 2 in MS is planned. This study illustrates the advantage of repurposing strategies allowing a phase 2 clinical trial only 2 years after the first article reporting the remyelinating potential of the molecule.
40. Buckley CE, Marguerie A, Roach AG, et al. Drug reprofiling using zebrafish identifies novel compounds with potential pro-myelination effects. Neuropharmacology 2010; 59:149–159.
41. Kaya F, Mannioui A, Chesneau A, et al. Live imaging of targeted cell ablation in Xenopus: a new model to study demyelination and repair. J Neurosci 2012; 32:12885–12895.
42. Mannioui A, Azoyan L, Sekizar S, et al. Impact of siponimod on CNS remyelination in a transgenic Xenopus model. ECTRIMS-ACTRIMS (Boston) 2014.
43. Mi S, Miller RH, Tang W, et al. Promotion of central nervous system remyelination by induced differentiation of oligodendrocyte precursor cells. Ann Neurol 2009; 65:304–315.
44. Magalon K, Zimmer C, Cayre M, et al. Olesoxime accelerates myelination and promotes repair in models of demyelination. Ann Neurol 2012; 71:213–226.
45. Deshmukh VA, Tardif V, Lyssiotis CA, et al. A regenerative approach to the treatment of multiple sclerosis. Nature 2013; 502:327–332.
46. Reich DS, White R, Cortese IC, et al. Sample-size calculations for short-term proof-of-concept studies of tissue protection and repair in multiple sclerosis lesions via conventional clinical imaging. Mult Scler 2015; 21:1693–1704.
47. Vavasour IM, Laule C, Li DK, et al. Is the magnetization transfer ratio a marker for myelin in multiple sclerosis? J Magn Reson Imaging 2011; 33:713–718.
48. Brown RA, Narayanan S, Arnold DL. Segmentation of magnetization transfer ratio lesions for longitudinal analysis of demyelination and remyelination in multiple sclerosis. Neuroimage 2013; 66:103–109.
49. Brown RA, Narayanan S, Banwell B, et al. Magnetization transfer ratio recovery in new lesions decreases during adolescence in pediatric-onset multiple sclerosis patients. Neuroimage Clin 2014; 6:237–242.
50. Brown RA, Narayanan S, Arnold DL. Imaging of repeated episodes of demyelination and remyelination in multiple sclerosis. Neuroimage Clin 2014; 6:20–25.
51. Derakhshan M, Caramanos Z, Narayanan S, et al. Surface-based analysis reveals regions of reduced cortical magnetization transfer ratio in patients with multiple sclerosis: a proposed method for imaging subpial demyelination. Hum Brain Mapp 2014; 35:3402–3413.
52. Moll NM, Rietsch AM, Thomas S, et al. Multiple sclerosis normal-appearing white matter: pathology-imaging correlations. Ann Neurol 2011; 70:764– 773.
53. Turati L1, Moscatelli M, Mastropietro A, et al. In vivo quantitative magnetization transfer imaging correlates with histology during de- and remyelination in cuprizone-treated mice. NMR Biomed 2015; 28:327–337.
54. MacKay A, Laule C, Vavasour I, et al. Insights into brain microstructure from the T2 distribution. Magn Reson Imaging 2006; 24:515–525.
55. Meyers SM, Laule C, Vavasour IM, et al. Reproducibility of myelin water fraction analysis: a comparison of region of interest and voxel-based analysis methods. Magn Reson Imaging 2009; 27:1096–1103.
56. Vavasour IM, Laule C, Li DK, et al. Longitudinal changes in myelin water fraction in two MS patients with active disease. J Neurol Sci 2009; 276:49–53.
57. Levesque IR, Sled JG, Narayanan S, et al. Reproducibility of quantitative magnetization-transfer imaging parameters from repeated measurements. Magn Reson Med 2010; 64:391–400.
58. Kitzler HH, Su J, Zeineh M, et al. Deficient MWF mapping in multiple sclerosis using 3D whole-brain multicomponent relaxation MRI. Neuroimage 2012; 59:2670–2677.
59. Kolind S, Seddigh A, Combes A, et al. Brain and cord myelin water imaging: a progressive multiple sclerosis biomarker. Neuroimage Clin 2015; 9:574– 580.
60. Nguyen TD, Deh K, Monohan E, et al. Feasibility and reproducibility of whole brain myelin water mapping in 4 min using fast acquisition with spiral trajectory and adiabatic T2prep (FAST-T2) at 3T. Magn Reson Med 2015; 42:1592– 1600.
61. Raj A, Pandya S, Shen X, et al. Multicompartment T2 relaxometry using a spatially constrained multi-Gaussian model. PLoS One 2014; 9:e98391.
62. Fox RJ, Cronin T, Lin J, et al. Measuring myelin repair and axonal loss with diffusion tensor imaging. AJNR Am J Neuroradiol 2011; 32:85–91.
63. & Wang Y, Sun P, Wang Q, et al. Differentiation and quantification of inflammation, demyelination and axonal injury or loss in multiple sclerosis. Brain 2015; 138:1223–1238. A novel diffusion technique that models diffusion weighted signal as a linear combination of multiple tensors, discriminating between the anisotropic fibre component and a full range of isotropic components, enabling to differentiate inflammation and oedema from axonal and myelin damage in a mouse demyelinating model.
64. Guglielmetti C, Veraart J, Roelant E, et al. Diffusion kurtosis imaging probes cortical alterations and white matter pathology following cuprizone induced demyelination and spontaneous remyelination. Neuroimage 2016; 125:363– 377.
65. Falangola MF, Guilfoyle DN, Tabesh A, et al. Histological correlation of diffusional kurtosis and white matter modeling metrics in cuprizone-induced corpus callosum demyelination. NMR Biomed 2014; 27:948–957.
66. Yoshida M, Hori M, Yokoyama K, et al. Diffusional kurtosis imaging of normalappearing white matter in multiple sclerosis: preliminary clinical experience. Jpn J Radiol 2013; 31:50–55.
67. Stankoff B, Wang Y, Bottlaender M, et al. Imaging of CNS myelin by positronemission tomography. Proc Natl Acad Sci U S A 2006; 103:9304–9309.
68. Bajaj A, La Plante NE, Cotero VE, et al. Identification of the protein target of myelin-binding ligands by immunohistochemistry and biochemical analyses. J Histochem Cytochem 2013; 61:19–30.
69. Wang Y, Wu C, Caprariello A, et al. In vivo quantification of myelin changes in the vertebrate nervous system. J Neurosci 2009; 29:14663–14669.
70. Wu C, Zhu J, Baeslack J, et al. Longitudinal positron emission tomography imaging for monitoring myelin repair in the spinal cord. Ann Neurol 2013; 74:688–698.
71. De Paula F, Copray S, Sijbesma JW, et al. PET imaging of focal demyelination and remyelination in a rat model of multiple sclerosis: comparison of [11C]MeDAS, [11C]CIC and [11C]PIB. Eur J Nucl Med Mol Imaging 2014; 41:995– 1003.
72. Stankoff B, Freeman L, Aigrot MS, et al. Imaging central nervous system myelin by positron emission tomography in multiple sclerosis using [methyl- (1)(1)C]-2-(40 -methylaminophenyl)-6-hydroxybenzothiazole. Ann Neurol 2011; 69:673–680.
73. Veronese M, Bodini B, Garcı´a-Lorenzo D, et al. Quantification of [(11)C]PIB PET for imaging myelin in the human brain: a test-retest reproducibility study in high-resolution research tomography. J Cereb Blood Flow Metab 2015; 35:1771–1782.
74. && Bodini B, Veronese M, Garcia-Lorenzo D, et al. Dynamic imaging of individual remyelination profiles in multiple sclerosis. Ann Neurol 2016. [Epub ahead of print] A longitudinal study using positron emission tomography to assess myelin dynamics in white matter lesions during the relapsing phase of the multiple sclerosis. Patients were shown to be heterogeneous according to their individual remyelination potential, which in turn appeared to be highly correlated with neurological disability. This could provide a new prognostic index as well as a promising tool to monitor remyelination in therapeutic trials.
75. Matı´as-Guiu JA, Cabrera-Martı´n MN, Matı´as-Guiu J, et al. Amyloid PET imaging in multiple sclerosis: an (18)F-florbetaben study. BMC Neurol 2015; 15:243.
76. Altmann DR, Button T, Schmierer K, et al. Sample sizes for lesion magnetisation transfer ratio outcomes in remyelination trials for multiple sclerosis. Mult Scler Relat Disord 2014; 3:237–243.
77. Luessi F, Kuhlmann T, Zipp F. Remyelinating strategies in multiple sclerosis. Expert Rev Neurother 2014; 14:1315–1334.
78. Harlow DE, Honce JM, Miravalle AA. Remyelination therapy in multiple sclerosis. Front Neurol 2015; 6:257.



