Rehabilitation Interventions for the Management of Multiple Sclerosis Relapse
Why is this important to me?
If you have the relapsing-remitting form of MS, you are likely to experience a relapse every 1 to 2 years. Relapses are unpredictable and are characterized by worsening of symptoms or abilities lasting at least a day to several weeks. The most common treatment option for a relapse is administration of steroids. MS relapses result in residual disability in 34-58% of people, and drugs such as steroids will not change your level of disability. Rehabilitation likely plays a role in managing a relapse and in optimal recovery. Although not everyone who experiences a relapse will require rehabilitation, strategies in addition to drug therapy are needed to decrease residual disability after an MS relapse.
What is the objective of this study?
Rehabilitation is defined here as “an educational, problem-solving process that focuses on activity limitations and aims to optimize patient participation and well-being, and so reduce stress on career/family.” The authors reviewed rehabilitation strategies for treating relapses in people with MS. After performing a search of previously published studies on non-drug-related rehabilitation following an MS relapse, the authors identified three studies, all conducted in the United Kingdom, that they reviewed in more detail.
In all three studies, patients received rehabilitation services over the course of 3 to 18 days. These services were provided by an interdisciplinary team and included:
- Physical therapy, including passive stretching
- Occupational therapy
- Speech therapy
- Vocational therapy
- Psychotherapy
- Counseling from an MS nurse specialist, a neurologist, and an orthoptist (a professional who treats disorders of the eye and visual system)
- Health-promotion advice
- Bladder management for patients with incontinence
The interventions described in these three studies appeared to be effective for improving disability in patients with MS who experienced a relapse. However, the data for the effectiveness of non-drug interventions remain sparse. Factors that may be important to their effectiveness include patient education and self-management. In addition, whether these interventions can improve your ability to return to work, reduce fatigue, improve your walking ability, or affect other aspects of the disease. Another question is whether these rehabilitative services would be practical and affordable for patients in outpatient or home settings in the US. Researchers also need to explore further how much recovery occurs without rehabilitation services. Thus, further investigation is needed to understand what people need after an MS relapse, how to address those needs, what might prevent someone from receiving a needed intervention, and the timing of delivery of drug therapy in relation to delivery of non-drug interventions.
How did the authors study this issue?
The authors performed a search of previously published studies describing non-drug rehabilitation programs for people experiencing an MS relapse. They reviewed three studies that described the characteristics and effectiveness of these interventions, which collectively were used to treat 145 adults with an MS relapse.
| SHARE: | |||||
Original Article
Rehabilitation Interventions for the Management of Multiple Sclerosis Relapse
A Short Scoping Review
International Journal of MS Care
Miho Asano, PhD; Rebecca Raszewski, MS; Marcia Finlayson, PhD
Background: This review was undertaken to identify and summarize the existing evidence regarding post relapse rehabilitation interventions in people with multiple sclerosis (MS). Methods: Literature searches were conducted within the following databases: CINAHL Plus with Full Text, MEDLINE via Ovid, and PsycINFO via CSA Illumina. The following terms were searched as subject headings or keywords: choice behavior, counseling, decision making, disease management, health education, health promotion, patient education, patient participation, patient satisfaction, psychotherapy, rehabilitation, self-care, self-management. Then these searches were combined with the subject headings for relapsing-remitting multiple sclerosis and subject heading or keywords for recurrence/relapse. Through the initial database search and additional citation search, 260 potentially relevant citations were identified. After screening the titles and abstracts as well as the citation search results, the reviewers agreed to keep five studies for the full-text reviews. Three rehabilitation intervention studies were included in the final review.
Results: A combined total of 145 adults who experienced a relapse within the previous 5 months received 3 to 18 days of rehabilitation. All three studies suggested the benefit of multidisciplinary rehabilitation for individuals with MS to improve impairment or disability.
Conclusions: The three multidisciplinary rehabilitation interventions included in this review appear to be effective in improving impairment or disability of people with MS who experienced a relapse. Given the limited number of studies and their methodological limitations, the results must be interpreted cautiously. Further investigation is needed to better understand the rehabilitation needs of people with MS after relapse in order to improve research and care.
One of the hallmarks of multiple sclerosis (MS) is periodic and unpredictable relapses, which are characterized by an acute worsening of symptoms or function lasting at least 24 hours and up to several weeks.1,2 With the exception of the progressive type of MS, most people with MS experience periodic relapses every 1 to 2 years.3,4 According to the 2007 North American Research Committee on Multiple Sclerosis (NARCOMS) survey on relapse management, 34% of the respondents (n = 2435) experienced a relapse in the previous 6 months.5 The current practice of MS relapse care focuses on the use of pharmacologic agents (eg, steroids) as the immediate and common treatment option.6,7 Consequently, the majority of MS relapse management research is focused on examining the utility and/or effectiveness of these agents. According to a US study that estimated the cost of managing a relapse,8 approximately 10% of the cost of managing a moderate-to-severe relapse was spent on rehabilitation therapies. Despite the common use of pharmacologic agents, they do not change the residual level of disability. Some authors have reported that 34% to 58% of MS relapses leave some level of residual disability.9,10
Rehabilitation can be defined as “an educational, problem-solving process that focuses on activity limitations and aims to optimize patient participation and well-being, and so reduce stress on carer/family.”11 Several existing Cochrane systematic reviews suggest the positive impacts of rehabilitation on the health, fitness, and quality of life of people with MS.12-17 Considering these benefits, rehabilitation can potentially play an important role in managing MS relapses and facilitating the recovery process (eg, reducing the risk of long-term disability, providing strategies to manage residual disabilities, improving function toward prerelapse level).
In order to advance rehabilitation care and research in MS, it is important to understand the existing evidence for the post relapse rehabilitation interventions. A scoping review identifies and summarizes key concepts in a particular research area; it is a process of mapping the existing literature to find research gaps and make recommendations for future research.18-20
The goal of this short scoping review was to identify and summarize the existing evidence for post relapse rehabilitation interventions for the management of MS relapses. We aimed to answer the following two research questions: 1) What are the post relapse rehabilitation interventions presented in the literature? 2) How effective are the post relapse rehabilitation interventions in the management of MS relapses?
Methods
Search Strategy
Three literature searches were conducted within the following databases in May 2012: CINAHL Plus with Full Text, MEDLINE via Ovid, and PsycINFO via CSA Illumina. The search was updated between May and June 2013. Subject heading and keyword searches were performed, which varied slightly depending on the term mapping of the database. Similar subject headings and keywords were combined first using the Boolean operator “OR”. The following words were searched as subject headings and/or keywords: choice behavior, counseling, decision making, disease management, health education, health promotion, patient education, patient participation, patient satisfaction, psychotherapy, rehabilitation, recurrence, relapse, self-care, self-management. The subject headings for psychotherapy and rehabilitation were exploded, meaning that the searches included more specific kinds of therapies. Then subject headings and keywords from these searches were combined with the subject heading used in the database for relapsing-remitting multiple sclerosis, and the subject heading and keyword set for recurrence and relapse. To ensure that the initial searches were not missing any related studies, citation searches were conducted in: a) Web of Knowledge (1950 to date) for repeated authors (>3); and b) Cochrane Database of Systematic Reviews for completed systematic reviews.
Selection Criteria
Studies had to have clear inclusion criteria or information for people with MS who were experiencing or recovering from MS relapses. All types of nonpharmacologic rehabilitation interventions (eg, physical therapy, occupational therapy, speech therapy, vocational therapy, counseling, and psychotherapy) for facilitating the management of MS relapse were considered. Additional types of interventions considered for the review were health promotion or education interventions, self-care or self-management interventions, and home or workplace modification interventions. The focus of the review was not on examining whether the interventions reduced the incidence of future relapses. Therefore, studies that reported only the incidence of MS relapses during or after interventions as the target outcome were excluded from the review. There were no other limitations placed on the type of outcome measures (eg, self-administered questionnaires, performance-based tests). In addition, this review was not limited by type or design of the studies, but was limited to studies written in English and published in peer-reviewed journals. Other publication types such as abstracts, conference proceedings, editorials, book chapters, dissertations, and review articles were excluded.
A list of all citations was created based on the initial search. Two reviewers independently assessed the relevance of each citation by reviewing 260 titles and abstracts, creating a list of final selections, and then comparing the lists. When two reviewers disagreed on the selection, a senior or a third reviewer was consulted for the final decision.
Data Collection and Extraction
Study designs, characteristics of study participants, intervention contents, outcome measures, and intervention effects were extracted for the review. Two reviewers extracted the data together and resolved any disagreements through discussion.
We used a review form developed by the McMaster University Occupational Therapy Evidence-Based Practice Research Group21 for the data extraction. Additional MS-specific information was also extracted (eg, level of disability, years since diagnosis).
Data Analysis
When it was possible, we calculated effect size (ES) to assess intervention effects. There are different ways to calculate ES.22 Because this review included one randomized controlled study and two pre-post design studies with different outcomes, ES was calculated for the target outcomes per group (ie, ∆ [post-pre]/SD [pooled]) to facilitate comparisons across different studies. An ES value of 0.8 or greater is considered strong (large); 0.5 to 0.8 is considered moderate; 0.2 to 0.5 is considered weak (small).23,24 For the studies with proportional data, we calculated odds ratio (OR) to assess the intervention effect.25
Results
Number of Citations and Studies
A total of 260 potentially relevant citations were identified through the database search (June 2013). The reviewers excluded one citation, as they were able to obtain neither an abstract nor the article’s full text. Two hundred fifty-nine titles and abstracts were screened at this point. Reviewers agreed to exclude 255 citations and kept 4 citations for the full-text reviews. Approximately 40% of excluded citations included pharmacologic and immunologic studies. An additional 7% of excluded citations were related to the examination of risk factors and impacts of relapses. The rest of the excluded citations were mostly unrelated to relapses (eg, natural history of MS, longitudinal studies, diagnostic and measurement studies). The cited reference search using Web of Knowledge identified an additional ten citations to be screened; reviewers agreed to add one citation, leading to a total of five citations selected for the full-text review.
A total of five citations selected for the full-text review. Title, keyword, and abstract search using “multiple sclerosis” in the Cochrane Database of Systematic Reviews identified 65 reviews. Sixteen of the 65 reviews were identified as nonpharmacologic reviews. Of those, a total of eight reviews that appeared potentially relevant examined multidisciplinary rehabilitation,16 vocational rehabilitation,17 occupational therapy,15 memory rehabilitation,14 exercise therapy,13 psychological interventions,26 and neuropsychological rehabilitation.12 The tables of included interventions were examined manually in these eight reviews. As pointed out by Khan et al.,16 we found that criteria for relapse were not always defined in these studies. This review included only the intervention studies that clearly stated inclusion of people with MS who had experienced a relapse, which is considered different from the existing and relevant reviews. No discrepancy was found between the studies reported in the existing reviews and this review.
Through the full-text reviews of five citations, we identified three multidisciplinary rehabilitation intervention studies and two patient education intervention studies. Patient education was considered an important part of the rehabilitation process. However, the reviewers found that the content of the patient education program on MS relapse management was focused heavily on corticosteroid therapy. As a result, the two patient education intervention studies were excluded from further analysis.
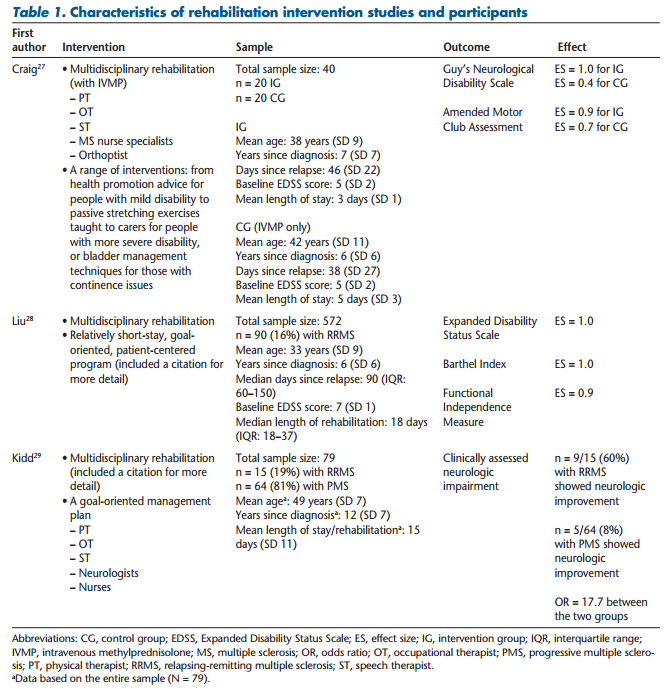
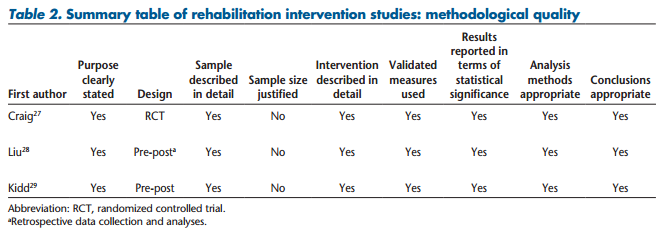
Study Designs, Interventions, Target Outcomes, and Participants
Of the three rehabilitation intervention studies involving people with MS who have experienced a relapse, one used a randomized controlled trial design27 and the other two used a pre-post design28,29 to assess the effect of rehabilitation interventions on disability and/or impairment.
The outcome measures used to evaluate the intervention effects included the Amended Motor Club Assessment (AMCA),27 Barthel Index (BI),28 Disability Status Scale (DSS),29 Expanded Disability Status Scale (EDSS),28 Functional Independence Measure (FIM),28 and Guy’s Neurological Disability Scale (GNDS),27 as well as a clinical assessment.
All three interventions were multidisciplinary rehabilitation (eg, physical therapy, occupational therapy, speech therapy, and sessions with an MS nurse specialist, a neurologist, and an orthoptist) offered at the hospitals where the studies were conducted. Two of the three interventions were carried out in an inpatient setting,28,29 and the remaining intervention was added to the steroid therapy (intravenous methylprednisolone; IVMP) among day case or inpatient patients who were treated for a relapse.27 From the literature, it was unclear whether these rehabilitation therapies were individual or group interventions. Depending on the study, the average length of rehabilitation intervention among participants ranged from 3 to 18 days.
The sample size (ie, participants with relapsing remitting MS [RRMS] receiving an intervention) ranged from 15 to 90 per group. The average ± SD age of participants ranged from 33 ± 9 years28 to 49 ± 7 years.29 The average ± SD time since the diagnosis ranged from 6 ± 6 years28 to 12 ± 7 years.29 Participants experienced a relapse up to 5 months prior to intervention. Tables 1 and 2 summarize the three rehabilitation intervention studies.
Intervention Effects
All three studies supported the benefit of multidisciplinary rehabilitation for people with MS, especially for those who experienced incomplete recovery from relapses with notable disability. The rehabilitation interventions showed strong ES values ranging from 0.9 (95% confidence interval [CI], 0.2-1.5) for AMCA27 to 1.0 for both the EDSS (95% CI, 0.3-1.7)28,29 and the BI (95% CI, 0.7-1.3).28 One study29 reported that 9 out of 15 participants with RRMS (60%) demonstrated neurologic improvement, whereas only 5 out of 64 participants with progressive MS (8%) who received the same intervention demonstrated the improvement. This result suggests that participants with RRMS who received the intervention are more likely to show neurologic improvement (OR, 17.7; 95% CI, 4.4-70.2) compared with those with progressive MS who received the same intervention.
Discussion
We found only three studies that investigated the effect of post relapse rehabilitation interventions in MS. All the studies were conducted in the United Kingdom and published over a decade ago. Given that the majority of research in MS relapse management focuses on the utility and/or effectiveness of pharmacologic agents, the limited number of studies found was not surprising at first. Nevertheless, because up to 58% of people with MS (based on published US data)9,10 may experience residual disabilities due to MS relapses, the small number of studies identified was disappointing. This made us ponder possible reasons for the lack of evidence—is it because rehabilitation is 1) not perceived as necessary for the management of MS relapse; 2) not considered part of standard MS relapse management; or 3) unavailable or unaffordable? Alternatively, is there a lack of awareness and/or knowledge among people with MS and/or their care providers about post relapse rehabilitation (eg, existence, availability, effectiveness)? These are important questions to be addressed in future studies to advance post relapse rehabilitation care in MS.
The search strategy or selection criteria were restricted by neither the types of limitations/disabilities caused by a relapse nor the country where the studies were conducted. However, given the limited number of studies found, a future review should consider a wider range of relevant terms (eg, home health, outpatient rehabilitation) as subject headings and keywords.
Rehabilitation positively affects functional abilities in various populations (eg, stroke, Parkinson’s disease, MS).13,30,31 Significant intervention effects on disability or impairment among people with MS reported in this review are consistent with research in other populations. However, an immediate apparent intervention effect after a relapse may simply be a result of natural recovery rather than rehabilitation. Future post relapse rehabilitation studies (whether observational or experimental) need to incorporate a control group and repeated outcome assessments over time to track the progress of recovery and estimate true intervention effects. Furthermore, the three interventions in this review appeared to be integrated into or added to standard hospital care in the United Kingdom, where the studies were conducted. Unfortunately, it is unclear whether these types of rehabilitation services would be feasible, effective, or affordable in non-inpatient settings (eg, outpatient, community, or home) or in North America. These are also important questions to explore in future studies.
Given the variability of MS relapses, comprehensive multidisciplinary rehabilitation approaches are likely necessary. All three studies in this review examined the impact of multidisciplinary rehabilitation interventions on impairments and/or disabilities. As a result, the outcome measures (eg, EDSS, BI, FIM) used to assess the intervention effects were as expected. However, as MS relapses can affect many different aspects of functioning, the use of a broader selection of outcome measures (eg, return to workforce, impact on fatigue, ability to walk, or use of resources to optimize recovery) should be considered for future studies. A qualitative study to understand how people with MS define their recovery from relapses and goals for their rehabilitation would also be valuable to determine appropriate outcomes and interventions for future studies.
The authors of one of the three studies27 stated that there is anecdotal evidence for a lack of adequate rehabilitation or education about appropriate care after discharge due to the timing of patients’ admission to steroid therapy. Timing and demands of therapies (whether steroids, rehabilitation, or education) can also be contributing factors in the lack of evidence for rehabilitation, and therefore they must also be explored in future studies.
When we looked for self-management, patient education, or health promotion programs in relapse management, we found two patient 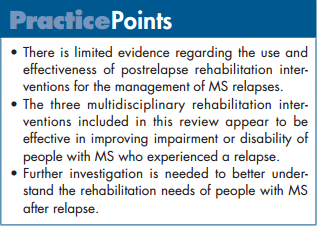 education interventions.32,33 While education on pharmacologic agents is important (given the effectiveness of these agents in reducing acute inflammation), these treatments have not been found effective in reducing long-term disability,34 which is the focus of rehabilitation. Because these two studies were primarily focused on the use and effect of pharmacologic agents, they were excluded from the review.
education interventions.32,33 While education on pharmacologic agents is important (given the effectiveness of these agents in reducing acute inflammation), these treatments have not been found effective in reducing long-term disability,34 which is the focus of rehabilitation. Because these two studies were primarily focused on the use and effect of pharmacologic agents, they were excluded from the review.
Not everyone who is experiencing or recovering from relapses will require rehabilitation; however, for those people who experience residual disability after relapse, it is important to establish which rehabilitation interventions can enable them to regain as much function as possible after the acute phase.
In summary, multidisciplinary rehabilitation interventions included in this review showed positive impacts on disability and impairment of people with MS who experienced a relapse. Despite the improvements found in the studies, the results must be interpreted cautiously because of their methodological limitations (eg, small sample size, lack of comparison groups). Further investigation is needed to better understand the rehabilitation needs of people with MS after relapse and potential barriers to the use of rehabilitation services during this time in order to improve MS research and care.
Acknowledgments: We thank Ms. Cleo Pappas, Associate Professor at the University of Illinois at Chicago, and Ms. Elizabeth Berg for their contributions to the review, as well as the University of Illinois at Chicago Library of Health Sciences and Department of Occupational Therapy for their support.
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: Dr. Asano’s time on this project was supported by a National Multiple Sclerosis Society postdoctoral training grant.
REFERENCES
1. Oleen-Burkey M, Castelli-Haley J, Lage MJ, Johnson KP. Burden of a multiple sclerosis relapse: the patient’s perspective. Patient. 2012;5:57–69.
2. Weinshenker BG, Bass B, Rice GP, et al. The natural history of multiple sclerosis: a geographically based study. I. Clinical course and disability. Brain. 1989;112(pt 1):133–146.
3. Kieseier BC, Stuve O. A critical appraisal of treatment decisions in multiple sclerosis—old versus new. Nat Rev Neurol. 2011;7:255–262.
4. Inusah S, Sormani MP, Cofield SS, et al. Assessing changes in relapse rates in multiple sclerosis. Mult Scler. 2010;16:1414–1421.
5. Tyry T. Relapse management. Mult Scler Q Rep. 2007;20–23.
6. Berkovich R. Treatment of acute relapses in multiple sclerosis. Neurotherapeutics. 2013;10:97–105.
7. Kopke S, Heesen C, Kasper J, Muhlhauser I. Steroid treatment for relapses in multiple sclerosis—the evidence urges shared decisionmaking. Acta Neurol Scand. 2004;110:1–5.
8. O’Brien JA, Ward AJ, Patrick AR, Caro J. Cost of managing an episode of relapse in multiple sclerosis in the United States. BMC Health Serv Res. 2003;3:17.
9. Leone MA, Bonissoni S, Collimedaglia L, et al. Factors predicting incomplete recovery from relapses in multiple sclerosis: a prospective study. Mult Scler. 2008;14:485–493.
10. Vercellino M, Romagnolo A, Mattioda A, et al. Multiple sclerosis relapses: a multivariable analysis of residual disability determinants. Acta Neurol Scand. 2009;119:126–130.
11. Wade DT. Describing rehabilitation interventions. Clin Rehabil. 2005;19:811–818.
12. Rosti-Otajarvi EM, Hamalainen PI. Neuropsychological rehabilitation for multiple sclerosis. Cochrane Database Syst Rev. 2011;11:CD009131.
13. Rietberg MB, Brooks D, Uitdehaag BM, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;1:CD003980.
14. das NR, Ferguson H, Stark DL, Lincoln NB. Memory rehabilitation for people with multiple sclerosis. Cochrane Database Syst Rev. 2012;3:CD008754.
15. Steultjens EM, Dekker J, Bouter LM, Cardol M, Van de Nes JC, Van den Ende CH. Occupational therapy for multiple sclerosis. Cochrane Database Syst Rev. 2003;3:CD003608.
16. Khan F, Turner-Stokes L, Ng L, Kilpatrick T. Multidisciplinary rehabilitation for adults with multiple sclerosis. Cochrane Database Syst Rev. 2007;2:CD006036.
17. Khan F, Ng L, Turner-Stokes L. Effectiveness of vocational rehabilitation intervention on the return to work and employment of persons with multiple sclerosis. Cochrane Database Syst Rev. 2009;1:CD007256.
18. Plow MA, Finlayson M, Rezac M. A scoping review of selfmanagement interventions for adults with multiple sclerosis. PM R. 2011;3:251–262.
19. Armstrong R, Hall BJ, Doyle J, Waters E. Cochrane Update. ‘Scoping the scope’ of a Cochrane review. J Public Health (Oxf). 2011;33: 147–150.
20. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
21. Law M, Steward D, Pollock N, Letts L, Bosch J, Westmorland M. Quantitative review form guidelines. 1998. http://www.srs-mcmaster.ca/ Default.aspx?tabid=630.
22. Durlak JA. How to select, calculate, and interpret effect sizes. J Pediatr Psychol. 2009;34:917–928. 23. Cohen J. A power primer. Psychol Bull. 1992;112:155–159.
24. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988.
25. Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol Res Pract. 2009;40:532–538.
26. Thomas PW, Thomas S, Hillier C, Galvin K, Baker R. Psychological interventions for multiple sclerosis. Cochrane Database Syst Rev. 2006;1:CD004431.
27. Craig J, Young CA, Ennis M, Baker G, Boggild M. A randomised controlled trial comparing rehabilitation against standard therapy in multiple sclerosis patients receiving intravenous steroid treatment. J Neurol Neurosurg Psychiatry. 2003;74:1225–1230.
28. Liu C, Playford ED, Thompson AJ. Does neurorehabilitation have a role in relapsing-remitting multiple sclerosis? J Neurol. 2003;250: 1214–1218.
29. Kidd D, Howard RS, Losseff NA, Thompson AJ. The benefit of in-patient neurorehabilitation. Clin Rehabil. 2013;9:198–203.
30. Gage H, Storey L. Rehabilitation for Parkinson’s disease: a systematic review of available evidence. Clin Rehabil. 2004;18:463–482.
31. Legg L, Langhorne P. Rehabilitation therapy services for stroke patients living at home: systematic review of randomised trials. Lancet. 2004;363:352–356.
32. Kopke S, Kasper J, Muhlhauser I, Nubling M, Heesen C. Patient education program to enhance decision autonomy in multiple sclerosis relapse management: a randomized-controlled trial. Mult Scler. 2009;15:96–104.
33. Kopke S, Richter T, Kasper J, Muhlhauser I, Flachenecker P, Heesen C. Implementation of a patient education program on multiple sclerosis relapse management. Patient Educ Couns. 2012;86:91–97.
34. Ontaneda D, Rae-Grant AD. Management of acute exacerbations in multiple sclerosis. Ann Indian Acad Neurol. 2009;12:264–272.
